Damage to healthy tissue is an unavoidable side effect of radiation therapy. The ability to deliver radiation from many different directions can help spare critical structures, but knowing which areas to avoid isn’t always obvious.
In the case of radiation therapy for lung cancer, the degree to which damage to healthy tissue will affect pulmonary function is hard to predict because high-functioning regions of the lung are not always the same among individuals due to effects of the disease.
Dr. John Bayouth, chief of radiation oncology physics and the Bhudatt Paliwal Professor of Human Oncology at the University of Wisconsin School of Medicine and Public Health, leads a clinical trial to study whether identifying and sparing individual patients’ high-ventilation regions of the lung will help preserve pulmonary function.
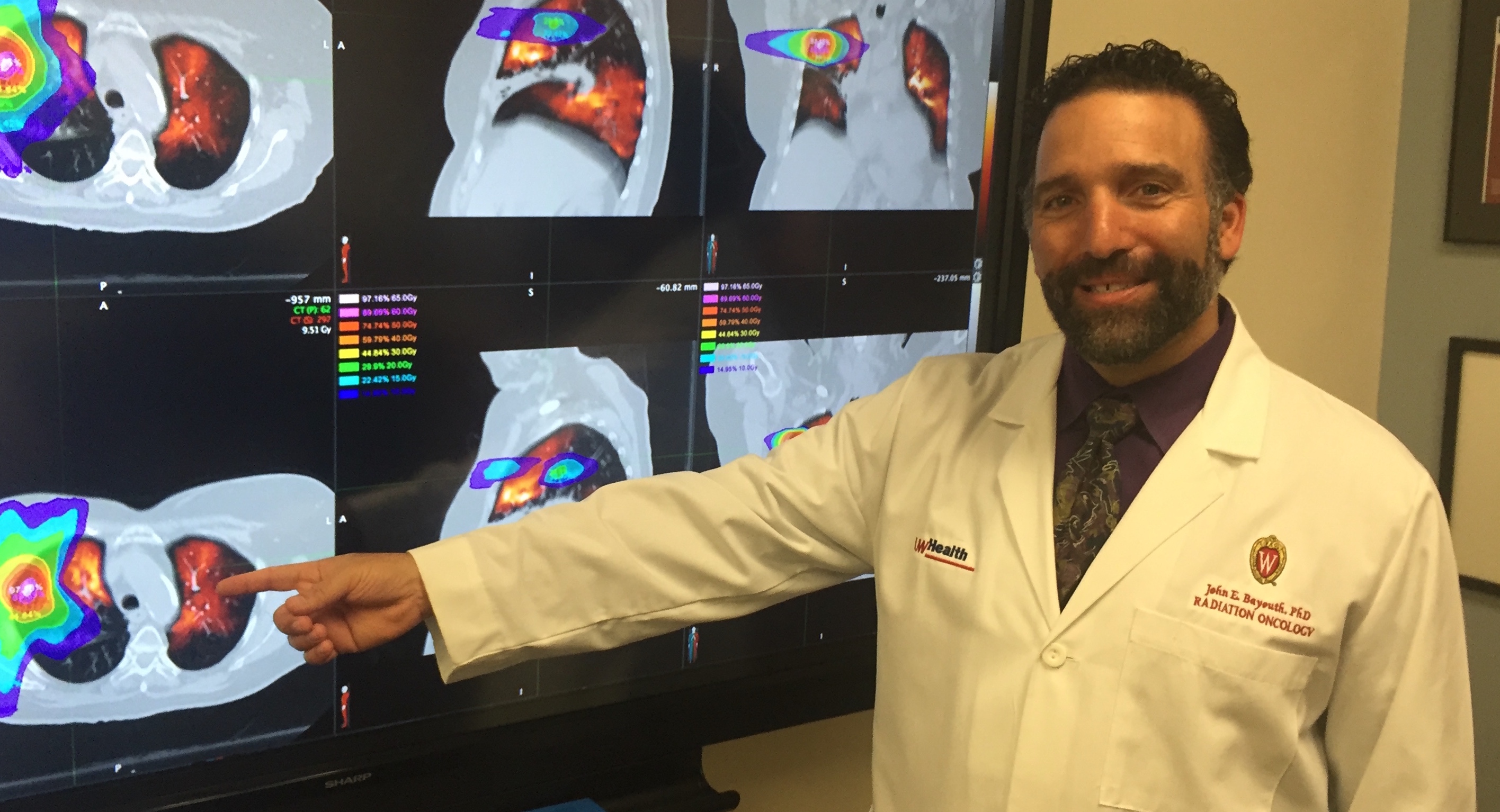
The trial consists of two arms of 60 patients each. Both arms receive four-dimensional CT (4DCT) scans, which provide full movies of patient breathing function. For patients in the treatment arm, these scans are used to calculate how each element of the lung expands during breathing, and these calculations are mathematically analyzed to predict how much lung damage will occur from the treatment. This information is then used to design treatment plans that might induce less damage to healthy lung regions. Patients in the control arm receive standard treatment, which does not incorporate the lung function information in treatment planning.
All the patients undergo additional 4DCT scans three, six and 12 months following treatment to measure the effects of the radiation on lung function. In addition, all the patients undergo pulmonary function testing before and after treatment and blood tests to measure inflammation, a marker of lung damage.
“Normal lung is even more sensitive to radiation than tumors are. This creates a problem when the tumor is surrounded by normal lung,” Bayouth says. “We are exploring techniques that help us see those lung regions that are functioning best and therefore may be ideal to avoid when delivering radiation. If we can limit radiation dose to high-functioning lung regions and allow radiation to pass through lesser-functioning lung regions, our hope is the patients will experience less long-term toxicity.”
This research could change the way radiation is prescribed for thoracic malignancies, says Dr. Andrew Baschnagel, DHO assistant professor, who, thus far, has enrolled the majority of patients for this clinical trial.
“Knowing which part of the lungs are high functioning would allow us to avoid damaging them with radiation,” Baschnagel says. “Currently, when planning radiation treatments, all lung tissue is considered to be equal. However, we know that is not the case. Anything we can do to spare and preserve lung function in patients who typically have poor lung function would be helpful. This technique being studied could also reduce a serious side effect of lung radiation known as radiation pneumonitis.”