In 2014, the radiation oncology clinic at the University of Wisconsin Hospital became one of the first sites in the world to begin treating patients using ViewRay MRIdian, an MRI-guided radiation therapy system. This system enables clinicians to monitor tumors and surrounding tissues during treatment to ensure accurate delivery of radiation. The department continues to lead in this area with its upgrade to a ViewRay MRIdian Linac, the only FDA-cleared radiation therapy system to combine MRI guidance with a linear accelerator (linac).
The system provides continuous high-contrast imaging of soft tissue to help clinicians place the patient for treatment, adapt treatment to changes in the patient’s anatomy, track tumor and normal organ motion and turn the beam on only when the tumor is precisely where it needs to be for optimal treatment.
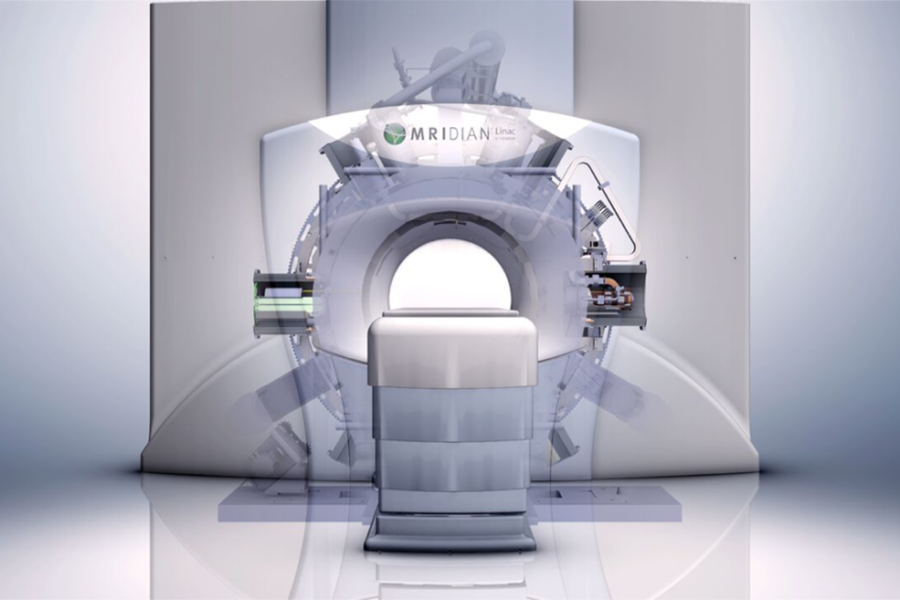
The upgrade to the MRIdian Linac provides several advantages. The X-rays produced by the linac have greater energy than the photons produced by the cobalt-60 sources and can more effectively penetrate tissues deep within the body. The linac version also provides a higher dose rate than cobalt-60, and its treatment beams provide a sharper penumbra to more closely adhere to the shape of the tumor and thereby minimize the dose to healthy structures.
“Having the sharp beam of the linac combined with the MRI visualization gives the ability to sculpt the dose more effectively,” says Dr. John Bayouth, professor of human oncology and chief of radiation oncology physics. “This may enable us to better address challenges that we’ve struggled with in the past in anatomical sites subject to motion and in close proximity to other organs. We’re excited to see where it might have the greatest impact.”
The linac will make possible more complex dose distributions in a shorter period of time. Less time on the treatment couch will likely improve the patient experience and could reduce the likelihood that the patient will move during treatment.
Thus far, UW clinicians have used MRI-guided radiotherapy to treat cancers of the breast, pancreas, liver, esophagus, stomach and kidney in more than 200 patients.
“The MRI-guided system has provided us with the first opportunity to actually see the treatment being delivered and modify it on the spot if we needed to,” says Dr. Bethany Anderson, assistant professor of human oncology. “Combining a linac with MRI guidance will provide sharp dose profiles and the ability to visualize and modify treatment as needed. It will be a fantastic resource that will likely benefit many patients.”
MRI guidance has been particularly useful in treating tumors in the thorax and abdomen, where significant motion takes place during normal processes such as respiration and digestion. By monitoring the MRI in real time, the clinician can instruct the patient to hold their breath to ensure that the treatment beam is on only when the tumor is in the correct position.
The upgrade to the MRIdian Linac enables more direct comparison of radiotherapy with and without MRI guidance. This will help researchers like Dr. Michael Bassetti, DHO assistant professor, better understand how MRI affects treatment outcomes and thereby help determine future clinical benefits.
Bassetti expects the upgrade to a linac to expand the use of MRI-guided radiotherapy to patients with central nervous system, head and neck, gynecological, prostate, rectal and anal cancers.
“The level of detail provided by this system gives us a lot of confidence in delivering high doses of radiation near structures that move or are very sensitive to radiation,” Bassetti says.
MRI-guided radiotherapy produces daily high-quality images that can be used to monitor anatomical changes and response to treatment. This provides useful guidance in treating patients. The data from these images could also be used in research to help predict outcomes and improve treatment of future patients.
“If we can tell from daily MRI scans that a patient’s tumor is shrinking, we may be able to use that information to predict whether or not that patient will have a complete response and adjust therapy to take advantage of that knowledge,” Bassetti says.
Bayouth notes that the University of Wisconsin has an extensive history of exploring how the amount of radiation dose given on a given day impacts a patient’s outcome. The same dose delivered in different fractions and at different intervals can affect the biological response to treatment.
“We’ve done a lot of work in this space,” Bayouth says. “On any given day, depending on anatomical changes, we may find we can safely deliver more radiation than we thought we could or need to give less radiation than we had planned. We’re going to be able to work with those parameters more intelligently than ever before and figure out ways to best deliver an effective dose to a tumor and minimize consequences to healthy surrounding tissues.”