Faculty and staff in the Department of Human Oncology at the University of Wisconsin School of Medicine and Public Health are investigating a new way to adjust radiation treatment plans rapidly to account for subtle anatomical changes that may occur daily during the course of treatment. This could help them more accurately deliver the prescribed radiation dose.
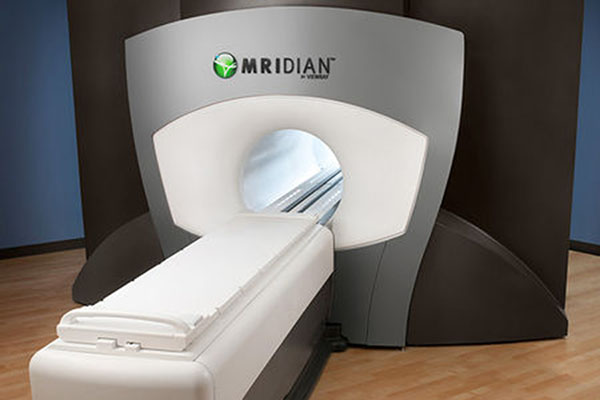
This new opportunity has emerged with the use of MRI-guided radiotherapy, using the ViewRay MRIdian machine to modify treatment plans during treatment. This technique, known as online adaptive radiotherapy, could reduce the amount of healthy tissue exposed to radiation and enable even higher radiation doses to be delivered to tumors.
The images of tumor and soft tissue captured by ViewRay before and during treatment enable clinicians to monitor the critical anatomy in real time and thereby “visualize” the precision delivery of radiation treatments. They can compare images taken during each daily treatment with images from the original treatment plan and revise these daily treatment plans on the fly.
“On a given treatment day there may be changes in tumor or normal organ positions. With this technique, we can now accurately predict how the original plan is affected by the patient’s current anatomy,” says Dr. Michael Bassetti, DHO assistant professor, who leads the department’s MRI-guided radiation therapy initiative. “Because the planning software is integrated with the delivery system, if these anatomical changes affect the radiation dose, then we are able to recognize this and rapidly adjust the treatment.”
This approach to online adaptive radiotherapy is made possible by the recent development of MRI-guided radiation therapy technology along with advances in computing power that originated in the video gaming industry. Calculations that used to take hours can now be completed in a few minutes. However, physicians still need to review and often manually adjust the organ contours for each new plan. This can take 20 to 30 minutes and may limit the types of patients for whom this approach is most valuable.
UW Health in Madison is one of just a few institutions in the world with a ViewRay MRIdian system. Bassetti has treated several patients using adaptive radiotherapy. He says that this technique will likely become more common as the department further develops standardized processes for its use and as research studies help determine which patients are most likely to benefit.
Bassetti and his colleagues have developed treatment protocols for this technique and are designing clinical trials to compare outcomes of patients whose treatment plans are adapted throughout treatment versus those whose plans remain constant.
Michael Bassetti, MD
Assistant Professor
“Online adaptive radiotherapy is a very important research arena in our field, and we have developed new procedures to do it safely and accurately. But will it make a significant difference clinically?” says Dr. John Bayouth, DHO professor and chief of radiation oncology physics. “Do patients have fewer toxicities when we redesign treatment plans on the fly? Does changing our treatment in response to changes seen within the patient improve tumor control? We’ve designed studies to answer these questions in our own department. And if online adaptive radiotherapy does improve outcomes, then we need to figure out if it’s scalable. Is it the knowledge of our radiation oncologists using our procedures for online adaptive radiotherapy that makes it effective, or can this be extended successfully beyond UW-Madison?”
Bassetti expects online adaptive radiotherapy may be used most extensively to treat gastrointestinal cancers because soft tissues in the abdomen are more clearly discernable with MR than with CT imaging. In addition, organs in the abdomen are subject to more motion than are organs in other parts of the body. Monitoring that motion and adjusting treatment as needed could improve patient outcomes.
A recent case illustrates the potential benefit of this technique. Bassetti used adaptive radiotherapy to treat a patient with gastroesophageal cancer. Treatment for this cancer typically includes irradiating the upper portion of the stomach. During one treatment session, the patient’s stomach had assumed a very different shape than during the original treatment plan. Had Bassetti used standard imaging—a CT scan once every few treatments—he may not have been aware of this change and the beam may have missed a portion of the target.
“This raises the question of how often this type of anatomic position and shape change is an issue,” Bassetti says. “It’s something we’re working to analyze as we accumulate more data.”
The ability to know with greater certainty that the radiation is precisely on target could enable clinicians to more safely deliver higher doses to tumors, which could improve outcomes for patients, including those with pancreatic cancer.
“We’re able to slow the local progression of many pancreatic cancers, but we’re not getting rid of the tumors, in part, because we cannot deliver enough dose to the tumor without harming the nearby intestine,” Bassetti says. “However, if we monitor the anatomy with even greater precision and adjust the treatment plan on a daily basis, we may be able to safely deliver a substantially larger dose and improve patient survival.”
Implementing online adaptive radiotherapy requires a strong commitment from the department and the larger UW Health enterprise. “It requires less effort to treat and not change the plan each day, but we are trying to improve outcomes and quality of life for future cancer patients,” Bassetti says. “We are fortunate to be at an institution that is willing to commit the time and resources to enable this type of groundbreaking work to move forward on behalf of the cancer patients we serve.”