I am a professor in the Department of Human Oncology specializing in treatment of breast and gynecologic cancers. In the clinic, my primary goal is to come alongside women and their families who are facing a cancer diagnosis and work together to identify a thoughtful treatment approach that best fits their cancer and life situation.
Through clinical research efforts, I strive to make radiation therapy an easier and more successful journey for women in the future. This includes the use of treatment methods that may be completed more quickly and/or limit radiation dose to nearby parts of the body. Accelerated partial breast irradiation (APBI), hypofractionated (short duration) whole breast irradiation, MRI-guided external radiation and brachytherapy are just a few examples of the treatment options that women may benefit from.
At the University of Wisconsin, I work with residents and medical students on a daily basis. I enjoy getting to know the trainees who come through the radiation oncology clinic, learning about their goals and helping them achieve those goals by building their clinical skills and research experience. Investing in bright, upcoming health care providers produces a ripple effect of caring and innovation, which can impact the future of medicine in a far greater way than the work of a single person.
Dr. Anderson's UW Health ProfileEducation
Fellow, Institut Gustave Roussy, Brachytherapy (2010)
Resident, University of Wisconsin–Madison, Radiation Oncology (2010)
MD, University of Wisconsin–Madison, Medicine (2005)
BA, Lawrence University, Biology and Biomedical Ethics (2001)
Academic Appointments
Professor (CHS), Human Oncology (2024)
Associate Professor (CHS), Human Oncology (2018)
Assistant Professor, Human Oncology (2010)
Selected Honors and Awards
Patient Experience Physician Champion Award, UW Health (2015)
Educator of the Year Award, ARRO (2013)
Boards, Advisory Committees and Professional Organizations
Committee for Equality Member, ASTRO (2017-pres.)
CME/MOC Committee Member, ASTRO (2015-pres.)
Corresponding Principal Investigator, NRG (2015-pres.)
Clinic Director, UW Radiation Oncology (2014-pres.)
Peer Review Committee Member, UW Health (2012-2014)
Research Focus
Breast Cancer, Gynecologic Cancer
Dr. Bethany Anderson specializes in the treatment of breast and gynecologic cancers. Her research is focused on partial breast irradiation, hypofractionated whole breast irradiation, MRI-guided external radiation and brachytherapy.
Traditional radiation therapy requires multiple treatments and may cause side effects in surrounding healthy tissues.
My research investigates ways to improve cancer control and reduce side effects of treatment for breast and gynecologic cancer. This includes using advanced imaging and radiation delivery techniques to more precisely identify and treat cancerous areas. I also study shorter treatment courses.
Magnetic Resonance Imaging (MRI)-Guided Breast Radiation
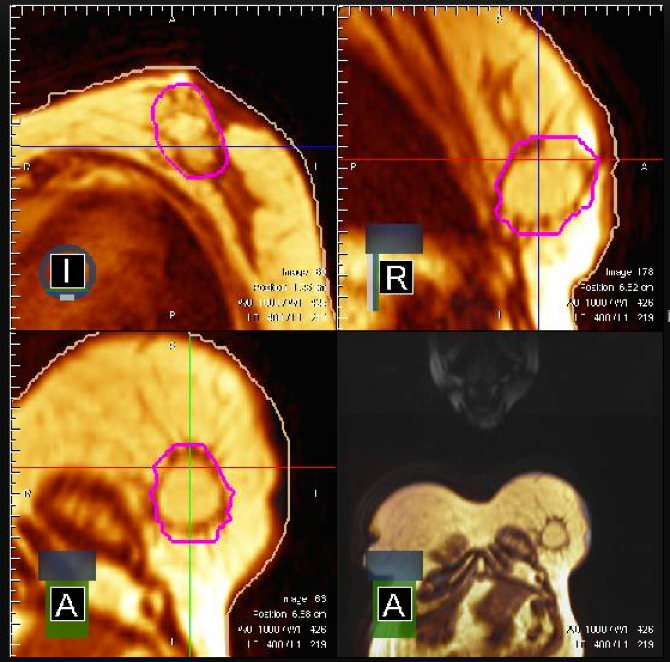
The University of Wisconsin is one of the first radiation oncology clinics in the world to offer treatment with the ViewRay treatment system. This allows us to monitor patients with MRI in real time before and during the delivery of radiation therapy, ensuring the most precise treatment possible. I am utilizing this technology to learn more about the motion of breast tissue (i.e., post-operative lumpectomy cavity) and other adjacent healthy organs (i.e., lung) between and during radiation treatments.
Accelerated Partial Breast Irradiation
Traditionally, nearly all women undergoing partial mastectomy for early-stage breast cancer received approximately six weeks of once-daily radiation treatments directed at the whole breast. Many options now exist that allow certain women to receive approximately one week of radiation treatments directed only to the portion of the breast affected by cancer (APBI). Soon, we will be offering women a novel option for receiving a total of three MRI-guided ViewRay APBI treatments precisely targeted to only the affected portion of the breast.
-
Benefit of clinical pharmacists in neurology clinics at an academic medical center Journal of the American Pharmacists Association : JAPhA
Anderson B, Snider MJ, Hansen M, Parks C, Bagnola A, Li J, Freimer M, Segal B
2003). 2024 Mar-Apr;64(2):492-498.e1. doi: 10.1016/j.japh.2024.01.010. Epub 2024 Jan 19.
-
More
BACKGROUND: Patients with neurologic diseases have complex medical needs and may benefit from the addition of clinical pharmacists in their care.
OBJECTIVES: This study aimed to describe integration and benefit of clinical pharmacists in neuroimmunology and neuromuscular clinics at an academic medical center.
METHODS: This retrospective chart review evaluated patients initiated on a neurology medication for a neuroimmunology or neuromuscular disease state before and after pharmacist integration in neurology clinics. The primary outcome measured access to an initially prescribed neuroimmunology or neuromuscular medication within 90 days of prescription. Secondary outcomes included access to an initially prescribed or alternative neurology medication owing to insurance requirements within 90 days, time from initial prescription to start, and description of pharmacist involvement.
RESULTS: There were 101 patients in the pregroup and 101 patients in the postgroup. The percentage of patients with confirmed initially prescribed medication access at 90 days increased in the postgroup compared with the pregroup (87.1% vs. 72.5%, respectively, P = 0.014). For secondary outcomes, the percentage of patients who started on an initially prescribed or alternative neuroimmunology or neuromuscular medication within 90 days also increased in the postgroup compared with the pregroup (90.0% vs. 73.3%, respectively, P = 0.004). Additional pharmacist involvement occurred in 64 patients (63.4%) in the postgroup and included prior authorization approval assistance, drug information support, and medication liaison interventions, with an average of 4.7 pharmacist interventions at each pharmacy-led encounter.
CONCLUSION: The addition of pharmacists into neuroimmunology and neuromuscular clinics improved operational access to medications for neuroimmunology and neuromuscular conditions. In addition, pharmacists were able to assist with multiple areas of patient care including medication education, monitoring, and serving as a medication liaison. This study supports continuing to offer clinical pharmacy services in neuroimmunology and neuromuscular departments and may support the addition of clinical pharmacists into neurology services at other institutions.
PMID:38246272 | DOI:10.1016/j.japh.2024.01.010
View details for PubMedID 38246272
-
More
-
Combinatorial Approaches for Chemotherapies and Targeted Therapies With Radiation: United Efforts to Innovate in Patient Care International journal of radiation oncology, biology, physics
Jabbour SK, Kumar R, Anderson B, Chino JP, Jethwa KR, McDowell L, Lo AC, Owen D, Pollom EL, Tree AC, Tsang DS, Yom SS
2024 Apr 1;118(5):1240-1261. doi: 10.1016/j.ijrobp.2024.01.010. Epub 2024 Jan 10.
-
More
Combinatorial therapies consisting of radiation therapy (RT) with systemic therapies, particularly chemotherapy and targeted therapies, have moved the needle to augment disease control across nearly all disease sites for locally advanced disease. Evaluating these important combinations to incorporate more potent therapies with RT will aid our understanding of toxicity and efficacy for patients. This article discusses multiple disease sites and includes a compilation of contributions from expert Red Journal editors from each disease site. Leveraging improved systemic control with novel agents, we must continue efforts to study novel treatment combinations with RT.
PMID:38216094 | DOI:10.1016/j.ijrobp.2024.01.010
View details for PubMedID 38216094
-
More
-
Empowering the Radiation Oncology Triage Nurse Role: A Single-Center Analysis Clinical journal of oncology nursing
Weber BW, Blitzer GC, Harari CM, Ruesga SL, Huenerberg KJ, Anderson B, Schuster JM
2023 Nov 16;27(6):637-643. doi: 10.1188/23.CJON.637-643.
-
More
BACKGROUND: Triage nurses play a crucial role in addressing patient telephone calls. However, topics that radiation oncology (RO) triage nurses encounter have not been thoroughly investigated.
OBJECTIVES: This project established baseline patient issues addressed via telephone by RO triage nurses in a clinically busy academic RO department; identified themes and potential areas for workflow improvement; and evaluated interprofessional perceptions of RO triage from nurses, physicians, and radiation therapists.
METHODS: This two-part study was conducted from September through November 2021 using a retrospective chart review that analyzed patient communications to the RO nurse triage line. Physicians, nurses, and radiation therapists completed an online survey about their experiences with nurse triage.
FINDINGS: Analysis revealed 13 message themes, with scheduling questions being the most common theme. Survey results indicated that average provider satisfaction with the effectiveness of triage was 3 of 5, perceived triage nurse preparedness to resolve encounters was 3 of 5, and perception of the triage program by physicians was 2.4 of 5.
PMID:38009877 | DOI:10.1188/23.CJON.637-643
View details for PubMedID 38009877
-
More
-
Publisher's Note to Partial Breast Irradiation for Patients With Early-Stage Invasive Breast Cancer or Ductal Carcinoma In Situ: An ASTRO Clinical Practice Guideline (Pract Radiat Oncol. 2024;14:xxx-xxx. Epub ahead of print November 14, 2023.) Practical radiation oncology
Shaitelman SF, Anderson BM, Arthur DW, Bazan JG, Bellon JR, Bradfield L, Coles CE, Gerber NK, Kathpal M, Kim L, Laronga C, Meattini I, Nichols EM, Pierce LJ, Poppe MM, Spears PA, Vinayak S, Whelan T, Lyons JA
2023 Nov 18:S1879-8500(23)00301-6. doi: 10.1016/j.prro.2023.11.005. Online ahead of print.
-
Partial Breast Irradiation for Patients With Early-Stage Invasive Breast Cancer or Ductal Carcinoma In Situ: An ASTRO Clinical Practice Guideline Practical radiation oncology
Shaitelman SF, Anderson BM, Arthur DW, Bazan JG, Bellon JR, Bradfield L, Coles CE, Gerber NK, Kathpal M, Kim L, Laronga C, Meattini I, Nichols EM, Pierce LJ, Poppe MM, Spears PA, Vinayak S, Whelan T, Lyons JA
2024 Mar-Apr;14(2):112-132. doi: 10.1016/j.prro.2023.11.001. Epub 2023 Nov 15.
-
More
PURPOSE: This guideline provides evidence-based recommendations on appropriate indications and techniques for partial breast irradiation (PBI) for patients with early-stage invasive breast cancer and ductal carcinoma in situ.
METHODS: ASTRO convened a task force to address 4 key questions focused on the appropriate indications and techniques for PBI as an alternative to whole breast irradiation (WBI) to result in similar rates of ipsilateral breast recurrence (IBR) and toxicity outcomes. Also addressed were aspects related to the technical delivery of PBI, including dose-fractionation regimens, target volumes, and treatment parameters for different PBI techniques. The guideline is based on a systematic review provided by the Agency for Healthcare Research and Quality. Recommendations were created using a predefined consensus-building methodology and system for grading evidence quality and recommendation strength.
RESULTS: PBI delivered using 3-dimensional conformal radiation therapy, intensity modulated radiation therapy, multicatheter brachytherapy, and single-entry brachytherapy results in similar IBR as WBI with long-term follow-up. Some patient characteristics and tumor features were underrepresented in the randomized controlled trials, making it difficult to fully define IBR risks for patients with these features. Appropriate dose-fractionation regimens, target volume delineation, and treatment planning parameters for delivery of PBI are outlined. Intraoperative radiation therapy alone is associated with a higher IBR rate compared with WBI. A daily or every-other-day external beam PBI regimen is preferred over twice-daily regimens due to late toxicity concerns.
CONCLUSIONS: Based on published data, the ASTRO task force has proposed recommendations to inform best clinical practices on the use of PBI.
PMID:37977261 | DOI:10.1016/j.prro.2023.11.001
View details for PubMedID 37977261
-
More
-
Concurrent Lapatinib With Brain Radiation Therapy in Patients With HER2+ Breast Cancer With Brain Metastases: NRG Oncology-KROG/RTOG 1119 Phase 2 Randomized Trial International journal of radiation oncology, biology, physics
Kim IA, Winter KA, Sperduto PW, Santos DL, Peereboom DM, Ogunleye T, Boulter D, Fritz JM, Cho KH, Shin KH, Zoberi I, Choi S, Palmer JD, Liem B, Kim YB, Anderson BM, Thakrar AW, Muanza TM, Kim MM, Choi DH, Mehta MP, White JR
2024 Apr 1;118(5):1391-1401. doi: 10.1016/j.ijrobp.2023.07.019. Epub 2023 Jul 26.
-
More
PURPOSE: Lapatinib plus whole brain radiation therapy (WBRT) or stereotactic radiosurgery (SRS) was hypothesized to improve the 12-week intracranial complete response (CR) rate compared with either option of radiation therapy (RT) alone for patients with brain metastases (BM) from human epidermal growth factor receptor 2-positive (HER2+) breast cancer.
METHODS AND MATERIALS: This study included patients with HER2+ breast cancer with ≥1 measurable, unirradiated BM. Patients were randomized to WBRT (37.5 Gy/3 wk)/SRS (size-based dosing) ± concurrent lapatinib (1000 mg daily for 6 weeks). Secondary endpoints included objective response rate (ORR), lesion-specific response, central nervous system progression-free survival, and overall survival.
RESULTS: From July 2012 to September 2019, 143 patients were randomized, with 116 analyzable for the primary endpoint. RT + lapatinib did not improve 12-week CR (0% vs 6% for RT alone, 1-sided P = .97), or ORR at 12 weeks. At 4 weeks, RT + lapatinib showed higher ORR (55% vs 42%). Higher graded prognostic assessment and ≤10 lesions were associated with higher 12-week ORR. Grade 3 and 4 adverse event rates were 8% and 0% for RT and 28% and 6% for RT + lapatinib.
CONCLUSIONS: The addition of 6 weeks of concomitant lapatinib to WBRT/SRS did not improve the primary endpoint of 12-week CR rate or 12-week ORR. Adding lapatinib to WBRT/SRS showed improvement of 4-week ORR, suggesting a short-term benefit from concomitant therapy.
PMID:37506981 | PMC:PMC10811275 | DOI:10.1016/j.ijrobp.2023.07.019
View details for PubMedID 37506981
-
More
-
NCCN Guidelines® Insights: Breast Cancer, Version 4.2023 Journal of the National Comprehensive Cancer Network : JNCCN
Gradishar WJ, Moran MS, Abraham J, Abramson V, Aft R, Agnese D, Allison KH, Anderson B, Burstein HJ, Chew H, Dang C, Elias AD, Giordano SH, Goetz MP, Goldstein LJ, Hurvitz SA, Jankowitz RC, Javid SH, Krishnamurthy J, Leitch AM, Lyons J, Mortimer J, Patel SA, Pierce LJ, Rosenberger LH, Rugo HS, Schneider B, Smith ML, Soliman H, Stringer-Reasor EM, Telli ML, Wei M, Wisinski KB, Young JS, Yeung K, Dwyer MA, Kumar R
2023 Jun;21(6):594-608. doi: 10.6004/jnccn.2023.0031.
-
More
The NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines) for Breast Cancer address all aspects of management for breast cancer. The treatment landscape of metastatic breast cancer is evolving constantly. The therapeutic strategy takes into consideration tumor biology, biomarkers, and other clinical factors. Due to the growing number of treatment options, if one option fails, there is usually another line of therapy available, providing meaningful improvements in survival. This NCCN Guidelines Insights report focuses on recent updates specific to systemic therapy recommendations for patients with stage IV (M1) disease.
PMID:37308117 | DOI:10.6004/jnccn.2023.0031
View details for PubMedID 37308117
-
More
-
Breast brachytherapy: Building a bright future on the foundation of a rich history of advancement in technology, technique, and patient-centered care Brachytherapy
Anderson B, Vicini F, Wazer D, Arthur D
2023 May-Jun;22(3):368-380. doi: 10.1016/j.brachy.2022.12.009. Epub 2023 Feb 3.
-
More
For over 20 years, the concept of accelerated partial breast irradiation (APBI) has received considerable attention. Initially concentrating on the appropriateness of APBI as an alternative treatment to whole breast radiotherapy, investigation and innovation evolved towards dose delivery and technique appropriateness. The purpose of this article is to review the pertinent literature that supports the role brachytherapy serves in delivering APBI and the recognized brachytherapy techniques for dose delivery. Publications establishing techniques utilizing multicatheter brachytherapy, single-entry brachytherapy applicators, permanent breast seed implantation brachytherapy, noninvasive breast brachytherapy and electronic brachytherapy are described. The use of brachytherapy for repeat breast conservation therapy is additionally reviewed. A historical perspective and potential direction of future investigation and innovation are presented.
PMID:36740541 | DOI:10.1016/j.brachy.2022.12.009
View details for PubMedID 36740541
-
More
-
Incidence of radiation-associated sarcoma after breast-conserving surgery plus radiation Journal of surgical oncology
Wiener AA, Schumacher JR, Hanlon B, Anderson B, Neuman HB
2023 Mar;127(4):535-540. doi: 10.1002/jso.27167. Epub 2022 Dec 7.
-
More
BACKGROUND: Radiation-associated sarcoma (RAS) is a rare sequela of radiotherapy. Radiotherapy modalities for breast conservation and radiation treatment (BCT) have changed over time. We sought to determine if the incidence of RAS after BCT has changed over time.
METHODS: We identified breast cancer survivors (diagnosed 1988-2012) treated with BCT within the SEER database. We excluded patients with prior cancer, <1-year follow-up/survival, and nonexternal beam radiation (n = 276 301). We identified patients with a subsequent chest sarcoma diagnosis. The primary predictor variable was a 5-year period of breast cancer diagnosis year (1988-1992, 1993-1997, etc.). The incidence of sarcoma was estimated by the Kaplan-Meier method, censoring at sarcoma diagnosis, death, or last follow-up (available through December 2017). Given the known latency of RAS, we used Joinpoint analysis to identify the time point at which RAS incidence significantly increased (start of the analytic window). A log-rank test assessed differences in RAS incidence by diagnosis year.
RESULTS: The incidence of RAS was 0.03% at 5 years (95% confidence interval [CI]: 0.03-0.04) and 0.16% at 10 years (95% CI: 0.14-0.18). No statistical difference in RAS incidence by diagnosis year was observed (p = 0.2).
CONCLUSIONS: RAS remains a rare but persistent sequela after BCT. As new radiation modalities become more common, ongoing surveillance is necessary to track these rare events.
PMID:36477419 | PMC:PMC11760338 | DOI:10.1002/jso.27167
View details for PubMedID 36477419
-
More
-
Partial breast irradiation: An updated consensus statement from the American brachytherapy society Brachytherapy
Anderson B, Arthur D, Hannoun-Levi J, Kamrava M, Khan A, Kuske R, Scanderbeg D, Shah C, Shaitelman S, Showalter T, Vicini F, Wazer D, Yashar C
2022 Nov-Dec;21(6):726-747. doi: 10.1016/j.brachy.2022.07.004. Epub 2022 Sep 15.
-
More
PURPOSE: In recent years, results with mature follow-up have been reported for several Phase III trials randomizing women to receive whole breast irradiation (WBI) versus varying modalities of partial breast irradiation (PBI). It is important to recognize that these methods vary in terms of volume of breast tissue treated, dose per fraction, and duration of therapy. As such, clinical and technical guidelines may vary among the various PBI techniques.
METHODS: Members of the American Brachytherapy Society with expertise in PBI performed an extensive literature review focusing on the highest quality data available for the numerous PBI options offered in the modern era. Data were evaluated for strength of evidence and published outcomes were assessed.
RESULTS: The majority of women enrolled on randomized trials of WBI versus PBI have been age >45 years with tumor size <3 cm, negative margins, and negative lymph nodes. The panel also concluded that PBI can be offered to selected women with estrogen receptor negative and/or Her2 amplified breast cancer, as well as ductal carcinoma in situ, and should generally be avoided in women with extensive lymphovascular space invasion.
CONCLUSIONS: This updated guideline summarizes published clinical trials of PBI methods. The panel also highlights the role of PBI for women facing special circumstances, such as history of cosmetic breast augmentation or prior breast irradiation, and discusses promising novel modalities that are currently under study, such as ultrashort and preoperative PBI. Updated consensus guidelines are also provided to inform patient selection for PBI and to characterize the strength of evidence to support varying PBI modalities.
PMID:36117086 | DOI:10.1016/j.brachy.2022.07.004
View details for PubMedID 36117086
-
More
-
Considering Lumpectomy Cavity PTV Expansions: Characterization of Intrafraction Lumpectomy Cavity Motion Practical radiation oncology
Merfeld EC, Blitzer GC, Kuczmarska-Haas A, Witt JS, Wojcieszynski AP, Mittauer KM, Hill PM, Bayouth JE, Yadav P, Anderson BM
2023 Jan-Feb;13(1):e14-e19. doi: 10.1016/j.prro.2022.08.011. Epub 2022 Sep 9.
-
More
PURPOSE: Accelerated partial breast irradiation and lumpectomy cavity boost radiation therapy plans generally use volumetric expansions from the lumpectomy cavity clinical target volume to the planning target volume (PTV) of 1 to 1.5 cm, substantially increasing the volume of irradiated breast tissue. The purpose of this study was to quantify intrafraction lumpectomy cavity motion during external beam radiation therapy to inform the indicated clinical target volume to PTV expansion.
METHODS AND MATERIALS: Forty-four patients were treated with a whole breast irradiation using traditional linear accelerator-based radiation therapy followed by lumpectomy cavity boost using magnetic resonance (MR)-guided radiation therapy on a prospective registry study. Two-dimensional cine-MR images through the center of the surgical cavity were acquired during each boost treatment to define the treatment position of the lumpectomy cavity. This was compared with the reference position to quantify intrafraction cavity motion. Free-breathing technique was used during treatment. Clinical outcomes including toxicity, cosmesis, and rates of local control were additionally analyzed.
RESULTS: The mean maximum displacement per fraction in the anterior-posterior (AP) direction was 1.4 mm. Per frame, AP motion was <5 mm in 92% of frames. The mean maximum displacement per fraction in the superior-inferior (SI) direction was 1.2 mm. Per frame, SI motion was <5 mm in 94% of frames. Composite motion was <5 mm in 89% of frames. Three-year local control was 97%. Eight women (18%) developed acute G2 radiation dermatitis. With a median follow-up of 32.4 months, cosmetic outcomes were excellent (22/44, 50%), good (19/44, 43%), and fair (2/44, 5%).
CONCLUSIONS: In approximately 90% of analyzed frames, intrafraction displacement of the lumpectomy cavity was <5 mm, with even less motion expected with deep inspiratory breath hold. Our results suggest reduced PTV expansions of 5 mm would be sufficient to account for lumpectomy cavity position, which may accordingly reduce late toxicity and improve cosmetic outcomes.
PMID:36089252 | DOI:10.1016/j.prro.2022.08.011
View details for PubMedID 36089252
-
More
-
Targeting the GTV in medically inoperable endometrial cancer using brachytherapy Brachytherapy
Merfeld EC, Kuczmarska-Haas A, Burr AR, Witt JS, Francis DM, Ntambi J, Desai VK, Huang JY, Miller JR, Lawless MJ, Wallace CR, Anderson BM, Bradley KA
2022 Nov-Dec;21(6):792-798. doi: 10.1016/j.brachy.2022.07.006. Epub 2022 Aug 24.
-
More
PURPOSE: We aimed to determine the relationship between gross tumor volume (GTV) dose and tumor control in women with medically inoperable endometrial cancer, and to demonstrate the feasibility of targeting a GTV-focused volume using imaged-guided brachytherapy.
METHODS AND MATERIALS: An endometrial cancer database was used to identify patients. Treatment plans were reviewed to determine doses to GTV, clinical target volume (CTV), and OARs. Uterine recurrence-free survival was evaluated as a function of CTV and GTV doses. Brachytherapy was replanned with a goal of GTV D98 EQD2 ≥ 80 Gy, without regard for coverage of the uninvolved uterus and while respecting OAR dose constraints.
RESULTS: Fifty-four patients were identified. In the delivered plans, GTV D90 EQD2 ≥ 80 Gy was achieved in 36 (81.8%) patients. Uterine recurrence-free survival was 100% in patients with GTV D90 EQD2 ≥ 80 Gy and 66.7% in patients with EQD2 < 80 Gy (p = 0.001). On GTV-only replans, GTV D98 EQD2 ≥ 80 Gy was achieved in 39 (88.6%) patients. Mean D2cc was lower for bladder (47.1 Gy vs. 73.0 Gy, p < 0.001), and sigmoid (47.0 Gy vs. 58.0 Gy, p = 0.007) on GTV-only replans compared to delivered plans. Bladder D2cc was ≥ 80 Gy in 11 (25.0%) delivered plans and four (9.1%) GTV-only replans (p = 0.043). Sigmoid D2cc was ≥ 65 Gy in 20 (45.4%) delivered plans and 10 (22.7%) GTV-only replans (p = 0.021).
CONCLUSIONS: OAR dose constraints should be prioritized over CTV coverage if GTV coverage is sufficient. Prospective evaluation of image-guided brachytherapy to a reduced, GTV-focused volume is warranted.
PMID:36030167 | DOI:10.1016/j.brachy.2022.07.006
View details for PubMedID 36030167
-
More
-
Breast Cancer, Version 3.2022, NCCN Clinical Practice Guidelines in Oncology Journal of the National Comprehensive Cancer Network : JNCCN
Gradishar WJ, Moran MS, Abraham J, Aft R, Agnese D, Allison KH, Anderson B, Burstein HJ, Chew H, Dang C, Elias AD, Giordano SH, Goetz MP, Goldstein LJ, Hurvitz SA, Isakoff SJ, Jankowitz RC, Javid SH, Krishnamurthy J, Leitch M, Lyons J, Mortimer J, Patel SA, Pierce LJ, Rosenberger LH, Rugo HS, Sitapati A, Smith KL, Smith ML, Soliman H, Stringer-Reasor EM, Telli ML, Ward JH, Wisinski KB, Young JS, Burns J, Kumar R
2022 Jun;20(6):691-722. doi: 10.6004/jnccn.2022.0030.
-
More
The therapeutic options for patients with noninvasive or invasive breast cancer are complex and varied. These NCCN Clinical Practice Guidelines for Breast Cancer include recommendations for clinical management of patients with carcinoma in situ, invasive breast cancer, Paget disease, phyllodes tumor, inflammatory breast cancer, and management of breast cancer during pregnancy. The content featured in this issue focuses on the recommendations for overall management of ductal carcinoma in situ and the workup and locoregional management of early stage invasive breast cancer. For the full version of the NCCN Guidelines for Breast Cancer, visit NCCN.org.
PMID:35714673 | DOI:10.6004/jnccn.2022.0030
View details for PubMedID 35714673
-
More
-
Improving the well-being of women with ductal carcinoma in situ: A worthy goal with an unclear route to success Cancer
Anderson BM, White JR
2022 Apr 15;128(8):1571-1573. doi: 10.1002/cncr.34125. Epub 2022 Feb 22.
-
De-escalating Locoregional Therapy for Axillary Micrometastases in Breast Cancer: How Much is Too Much? Clinical breast cancer
Merfeld EC, Burr AR, Brickson C, Neuman HB, Anderson BM
2022 Jun;22(4):336-342. doi: 10.1016/j.clbc.2022.01.001. Epub 2022 Jan 12.
-
More
BACKGROUND: The applicability of modern prospective data on adjuvant radiotherapy (RT) fields in patients with micrometastases is limited because many trials occurred prior to routine measurement of nodal metastasis size and modern sentinel lymph node evaluation techniques. We aimed to determine prognostic factors for patients with micrometastases and evaluate the impact of adjuvant RT on disease outcomes.
PATIENTS AND METHODS: Patients diagnosed with pathologic T1-T3 N1mi breast cancers between 2004-2015 were identified. Cox proportional hazards methods were used to determine characteristics predictive of locoregional recurrence (LRR). Tumor and treatment-specific factors were further evaluated using log-rank statistics to compare rates of LRR-free survival.
RESULTS: This analysis included 156 patients. On multivariable analysis, grade 3 histology (HR 10.84, 95% CI 2.72-43.21) and adjuvant RT (HR 0.22, 95% CI 0.06-0.81) were independent predictors of LRR. Among patients with grade 1-2 histology, 5-year LRR-free survival was 98.8% in patients who received adjuvant RT versus 100% in patients who did not receive adjuvant RT (P = .82). Among patients with grade 3 histology, 5-year LRR-free survival was 90.1% in patients who received adjuvant RT versus 53.0% in patients who did not receive adjuvant RT (P = .025), and 100% in patients receiving comprehensive nodal irradiation versus 76.7% in patients receiving whole breast irradiation or no RT (P = .045).
CONCLUSION: Patients with grade 3 micrometastases are at substantial risk for LRR. Adjuvant RT, including comprehensive nodal irradiation, should be strongly considered in these women.
PMID:35105500 | DOI:10.1016/j.clbc.2022.01.001
View details for PubMedID 35105500
-
More
-
Cathepsin S Evokes PAR<sub>2</sub>-Dependent Pain in Oral Squamous Cell Carcinoma Patients and Preclinical Mouse Models Cancers
Tu NH, Inoue K, Chen E, Anderson BM, Sawicki CM, Scheff NN, Tran HD, Kim DH, Alemu RG, Yang L, Dolan JC, Liu CZ, Janal MN, Latorre R, Jensen DD, Bunnett NW, Edgington-Mitchell LE, Schmidt BL
2021 Sep 19;13(18):4697. doi: 10.3390/cancers13184697.
-
More
Oral squamous cell carcinoma (SCC) pain is more prevalent and severe than pain generated by any other form of cancer. We previously showed that protease-activated receptor-2 (PAR2) contributes to oral SCC pain. Cathepsin S is a lysosomal cysteine protease released during injury and disease that can activate PAR2. We report here a role for cathepsin S in PAR2-dependent cancer pain. We report that cathepsin S was more active in human oral SCC than matched normal tissue, and in an orthotopic xenograft tongue cancer model than normal tongue. The multiplex immunolocalization of cathepsin S in human oral cancers suggests that carcinoma and macrophages generate cathepsin S in the oral cancer microenvironment. After cheek or paw injection, cathepsin S evoked nociception in wild-type mice but not in mice lacking PAR2 in Nav1.8-positive neurons (Par2Nav1.8), nor in mice treated with LY3000328 or an endogenous cathepsin S inhibitor (cystatin C). The human oral SCC cell line (HSC-3) with homozygous deletion of the gene for cathepsin S (CTSS) with CRISPR/Cas9 provoked significantly less mechanical allodynia and thermal hyperalgesia, as did those treated with LY3000328, compared to the control cancer mice. Our results indicate that cathepsin S is activated in oral SCC, and that cathepsin S contributes to cancer pain through PAR2 on neurons.
PMID:34572924 | PMC:PMC8466361 | DOI:10.3390/cancers13184697
View details for PubMedID 34572924
-
More
-
Improved Ipsilateral Breast and Chest Wall Sparing With MR-Guided 3-fraction Accelerated Partial Breast Irradiation: A Dosimetric Study Comparing MR-Linac and CT-Linac Plans Advances in radiation oncology
Musunuru HB, Yadav P, Olson SJ, Anderson BM
2021 Jan 22;6(3):100654. doi: 10.1016/j.adro.2021.100654. eCollection 2021 May-Jun.
-
More
PURPOSE: External beam accelerated partial breast irradiation (APBI) is subject to treatment uncertainties that must be accounted for through planning target volume (PTV) margin. We hypothesize that magnetic resonance-guided radiation therapy with reduced PTV margins enabled by real-time cine magnetic resonance image (MRI) target monitoring results in better normal tissue sparing compared with computed tomography (CT)-guided radiation therapy with commonly used clinical PTV margins. In this study, we compare the plan quality of ViewRay MRIdian Linac forward planned intensity modulated radiation therapy and TrueBeam volumetric modulated arc therapy for a novel 3-fraction APBI schedule.
METHODS AND MATERIALS: Targets and organs at risk (OARs) were segmented for 10 patients with breast cancer according to NSABP B39/RTOG 0413 protocol. A 3 mm margin was used to generate MR PTV3mm and CT PTV3mm plans, and a 10 mm margin was used for CT PTV10mm. An APBI schedule delivering 24.6 Gy to the clinical target volume and 23.4 Gy to the PTV in 3 fractions was used. OAR dose constraints were scaled down from existing 5-fraction APBI protocols. Target and OAR dose-volume metrics for the following data sets were analyzed using Wilcoxon matched-pairs signed-rank test: (1) MR PTV3mm versus CT PTV3mm plans and (2) MR PTV3mm versus CT PTV10mm.
RESULTS: Average PTVs were 84.3 ± 51.9 cm3 and 82.6 ± 55 cm3 (P = .5) for MR PTV3mm and CT PTV3mm plans, respectively. PTV V23.4Gy, dose homogeneity index, conformity index (CI), and R50 were similar. There was no meaningful difference in OAR metrics, despite MR PTV3mm being larger than the CT PTV3mm in 70% of the patients. Average PTVs for MR PTV3mm and CT PTV10mm plans were 84.3 ± 51.9 cm3 and 131.7 ± 74.4 cm3, respectively (P = .002). PTV V23.4Gy was 99% ± 0.9% versus 97.6% ± 1.4% (P = .03) for MR PTV3mm and CT PTV10mm, respectively. Dose homogeneity index, CI, and R50 were similar. MR PTV3mm plans had better ipsilateral breast (V12.3Gy, 34.8% ± 12.7% vs 44.4% ± 10.9%, P = .002) and chest wall sparing (V24Gy, 8.5 ± 5.5 cm3 vs 21.8 ± 14.9 cm3, P = .004).
CONCLUSIONS: MR- and CT-based planning systems produced comparable plans when a 3 mm PTV margin was used for both plans. As expected, MR PTV3mm plans produced better ipsilateral breast and chest wall sparing compared with CT PTV10mm. The clinical relevance of these differences in dosimetric parameters is not known.
PMID:34195491 | PMC:PMC8233460 | DOI:10.1016/j.adro.2021.100654
View details for PubMedID 34195491
-
More
-
Late Radiation Related Brachial Plexopathy After Pulsed Reduced Dose Rate Reirradiation of an Axillary Breast Cancer Recurrence Practical radiation oncology
Morris BA, Burr AR, Anderson BM, Howard SP
2021 Sep-Oct;11(5):319-322. doi: 10.1016/j.prro.2021.06.003. Epub 2021 Jun 24.
-
More
Radiation induced brachial plexopathy (RIBP) is an unfortunate complication of radiation involving the axilla and supraclavicular fossa. This case report highlights development of RIBP in a patient 15 years after initial radiation and 11 years after pulsed low dose rate (PRDR) re-irradiation for recurrent disease. PRDR is a radiation technique believed to lower normal tissue toxicity due to improved sublethal intrafraction damage repair of these tissues at low radiation dose rates with good reported long term locoregional control in the re-irradiation setting. However, RIBP, as seen in this patient, is a devastating side effect of high dose radiation to this region, with no effective treatment options outside of symptom management and control. In this case, the patient has remained disease free following her recurrence but has had continued RIBP with minimal improvement using pentoxyfilline for management.
PMID:34171539 | DOI:10.1016/j.prro.2021.06.003
View details for PubMedID 34171539
-
More
-
Concurrent Radiation and Modern Systemic Therapies for Breast Cancer: An Ever-Expanding Frontier Clinical breast cancer
Witt JS, Wisinski KB, Anderson BM
2021 Apr;21(2):120-127. doi: 10.1016/j.clbc.2020.11.019.
-
More
Radiotherapy is a critical tool for reducing locoregional recurrence, extending survival, and palliating symptoms in patients with breast cancer. With an ever-expanding armamentarium of systemic agents available, and an increasing trend toward the use of hypofractionated radiation regimens, it can be difficult to determine the safety of concurrent therapy. In particular, new targeted agents in both the adjuvant and metastatic setting have limited prospective or long-term data demonstrating safety when delivered concurrently with radiotherapy. Other systemic agents, including chemotherapy and endocrine therapy, are also important components of the overall treatment strategy for localized and metastatic breast cancer, and are often delivered concurrently with radiation in certain clinical scenarios. This review explores the safety, efficacy, and pitfalls of delivering radiation in conjunction with systemic therapies for breast cancer.
PMID:34030859 | DOI:10.1016/j.clbc.2020.11.019
View details for PubMedID 34030859
-
More
-
Legumain Induces Oral Cancer Pain by Biased Agonism of Protease-Activated Receptor-2 The Journal of neuroscience : the official journal of the Society for Neuroscience
Tu NH, Jensen DD, Anderson BM, Chen E, Jimenez-Vargas NN, Scheff NN, Inoue K, Tran HD, Dolan JC, Meek TA, Hollenberg MD, Liu CZ, Vanner SJ, Janal MN, Bunnett NW, Edgington-Mitchell LE, Schmidt BL
2021 Jan 6;41(1):193-210. doi: 10.1523/JNEUROSCI.1211-20.2020. Epub 2020 Nov 10.
-
More
Oral squamous cell carcinoma (OSCC) is one of the most painful cancers, which interferes with orofacial function including talking and eating. We report that legumain (Lgmn) cleaves protease-activated receptor-2 (PAR2) in the acidic OSCC microenvironment to cause pain. Lgmn is a cysteine protease of late endosomes and lysosomes that can be secreted; it exhibits maximal activity in acidic environments. The role of Lgmn in PAR2-dependent cancer pain is unknown. We studied Lgmn activation in human oral cancers and oral cancer mouse models. Lgmn was activated in OSCC patient tumors, compared with matched normal oral tissue. After intraplantar, facial or lingual injection, Lgmn evoked nociception in wild-type (WT) female mice but not in female mice lacking PAR2 in NaV1.8-positive neurons (Par2Nav1.8), nor in female mice treated with a Lgmn inhibitor, LI-1. Inoculation of an OSCC cell line caused mechanical and thermal hyperalgesia that was reversed by LI-1. Par2Nav1.8 and Lgmn deletion attenuated mechanical allodynia in female mice with carcinogen-induced OSCC. Lgmn caused PAR2-dependent hyperexcitability of trigeminal neurons from WT female mice. Par2 deletion, LI-1, and inhibitors of adenylyl cyclase or protein kinase A (PKA) prevented the effects of Lgmn. Under acidified conditions, Lgmn cleaved within the extracellular N terminus of PAR2 at Asn30↓Arg31, proximal to the canonical trypsin activation site. Lgmn activated PAR2 by biased mechanisms in HEK293 cells to induce Ca2+ mobilization, cAMP formation, and PKA/protein kinase D (PKD) activation, but not β-arrestin recruitment or PAR2 endocytosis. Thus, in the acidified OSCC microenvironment, Lgmn activates PAR2 by biased mechanisms that evoke cancer pain.SIGNIFICANCE STATEMENT Oral squamous cell carcinoma (OSCC) is one of the most painful cancers. We report that legumain (Lgmn), which exhibits maximal activity in acidic environments, cleaves protease-activated receptor-2 (PAR2) on neurons to produce OSCC pain. Active Lgmn was elevated in OSCC patient tumors, compared with matched normal oral tissue. Lgmn evokes pain-like behavior through PAR2 Exposure of pain-sensing neurons to Lgmn decreased the current required to generate an action potential through PAR2 Inhibitors of adenylyl cyclase and protein kinase A (PKA) prevented the effects of Lgmn. Lgmn activated PAR2 to induce calcium mobilization, cAMP formation, and activation of protein kinase D (PKD) and PKA, but not β-arrestin recruitment or PAR2 endocytosis. Thus, Lgmn is a biased agonist of PAR2 that evokes cancer pain.
PMID:33172978 | PMC:PMC7786216 | DOI:10.1523/JNEUROSCI.1211-20.2020
View details for PubMedID 33172978
-
More
-
Development and Implementation of an Algorithm to Guide MRI Screening in Patients With a Personal History of Treated Breast Cancer Clinical breast cancer
Strigel RM, Bravo E, Tevaarwerk AJ, Anderson BM, Stella AL, Neuman HB
2021 Feb;21(1):26-30. doi: 10.1016/j.clbc.2020.01.005. Epub 2020 Oct 17.
-
More
INTRODUCTION: Limited data exist to guide appropriate use of magnetic resonance imaging (MRI) screening in women with a personal history of breast cancer. We developed an algorithm to inform the use of MRI screening in patients with a personal history, implemented it, and evaluated initial implementation at our community and academic practice sites.
PATIENTS AND METHODS: A multidisciplinary committee of providers developed the initial algorithm on the basis of available literature and consensus. To evaluate projected MRI utilization based on the initial algorithm and inform algorithm revision, charts of patients < 80 years of age diagnosed and treated in 2010 with stage 0-III breast cancer (n = 236) were reviewed. The revised algorithm was implemented into the electronic medical record (September 2013). Thirteen months after implementation (2014-2015), chart review of patients with a personal history of breast cancer who underwent screening MRI was performed to assess algorithm adherence.
RESULTS: Before algorithm development, 9% (20/236) of patients received MRI screening (6 genetic mutation/family history, 4 occult primary, 8 young age/breast density, 2 unknown). Use of MRI screening was projected to increase to 25% with algorithm implementation. In postimplementation review, we identified 183 patients with a personal history of breast cancer who underwent screening MRI, with 94% algorithm adherence.
CONCLUSION: We successfully developed and implemented an algorithm to guide MRI screening in patients with a personal breast cancer history. Clinicians can use this algorithm to guide patient discussions regarding the utility of MRI screening. Further prospective study, including cancer detection rates, biopsy rate, and mortality, are necessary to confirm the algorithm's usefulness.
PMID:33162349 | PMC:PMC8812335 | DOI:10.1016/j.clbc.2020.01.005
View details for PubMedID 33162349
-
More
-
Does persistent use of radiation in women > 70 years of age with early-stage breast cancer reflect tailored patient-centered care? Breast cancer research and treatment
Taylor LJ, Steiman JS, Anderson B, Schumacher JR, Wilke LG, Greenberg CC, Neuman HB
2020 Apr;180(3):801-807. doi: 10.1007/s10549-020-05579-5. Epub 2020 Mar 3.
-
More
PURPOSE: Randomized controlled trials demonstrate that omission of radiation therapy (RT) in older women with early-stage cancer undergoing breast conserving surgery (BCS) is an "acceptable choice." Despite this, high RT rates have been reported. The objective was to evaluate the impact of patient- and system-level factors on RT rates in a contemporary cohort.
METHODS: Through the National Cancer Data Base, we identified women with clinical stage I estrogen receptor-positive breast cancer who underwent BCS (n = 84,214). Multivariable logistic regression identified patient, tumor, and system-level factors associated with RT. Joinpoint regression analysis calculated trends in RT use over time stratified by age and facility-type, reporting annual percent change (APC).
RESULTS: RT rates decreased from 2004 (77.2%) to 2015 (64.3%). The decline occurred earliest and was most pronounced in older women treated at academic facilities. At academic facilities, the APC was - 5.6 (95% CI - 8.6, - 2.4) after 2009 for women aged > 85 years, - 6.4 (95% CI - 9.0, - 3.8) after 2010 for women aged 80 - < 85 years, - 3.7 (95% CI - 5.6, - 1.9) after 2009 for women aged 75 - < 80, and - 2.4 (95% CI, - 3.1, - 1.6) after 2009 for women aged 70 - < 75. In contrast, at community facilities rates of RT declined later (2011, 2012, and 2013 for age groups 70-74, 75-79, and 80-84 years).
CONCLUSIONS: RT rates for older women with early-stage breast cancer are declining with patient-level variation based on factors related to life expectancy and locoregional recurrence. Facility-level variation suggests opportunities to improve care delivery by focusing on barriers to de-implementation of routine use of RT.
PMID:32125557 | PMC:PMC7474974 | DOI:10.1007/s10549-020-05579-5
View details for PubMedID 32125557
-
More
-
Hippocampal Avoidance During Whole-Brain Radiotherapy Plus Memantine for Patients With Brain Metastases: Phase III Trial NRG Oncology CC001 Journal of clinical oncology : official journal of the American Society of Clinical Oncology
Brown PD, Gondi V, Pugh S, Tome WA, Wefel JS, Armstrong TS, Bovi JA, Robinson C, Konski A, Khuntia D, Grosshans D, Benzinger LS, Bruner D, Gilbert MR, Roberge D, Kundapur V, Devisetty K, Shah S, Usuki K, Anderson BM, Stea B, Yoon H, Li J, Laack NN, Kruser TJ, Chmura SJ, Shi W, Deshmukh S, Mehta MP, Kachnic LA, Oncology fN
2020 Apr 1;38(10):1019-1029. doi: 10.1200/JCO.19.02767. Epub 2020 Feb 14.
-
More
PURPOSE: Radiation dose to the neuroregenerative zone of the hippocampus has been found to be associated with cognitive toxicity. Hippocampal avoidance (HA) using intensity-modulated radiotherapy during whole-brain radiotherapy (WBRT) is hypothesized to preserve cognition.
METHODS: This phase III trial enrolled adult patients with brain metastases to HA-WBRT plus memantine or WBRT plus memantine. The primary end point was time to cognitive function failure, defined as decline using the reliable change index on at least one of the cognitive tests. Secondary end points included overall survival (OS), intracranial progression-free survival (PFS), toxicity, and patient-reported symptom burden.
RESULTS: Between July 2015 and March 2018, 518 patients were randomly assigned. Median follow-up for alive patients was 7.9 months. Risk of cognitive failure was significantly lower after HA-WBRT plus memantine versus WBRT plus memantine (adjusted hazard ratio, 0.74; 95% CI, 0.58 to 0.95; P = .02). This difference was attributable to less deterioration in executive function at 4 months (23.3% v 40.4%; P = .01) and learning and memory at 6 months (11.5% v 24.7% [P = .049] and 16.4% v 33.3% [P = .02], respectively). Treatment arms did not differ significantly in OS, intracranial PFS, or toxicity. At 6 months, using all data, patients who received HA-WBRT plus memantine reported less fatigue (P = .04), less difficulty with remembering things (P = .01), and less difficulty with speaking (P = .049) and using imputed data, less interference of neurologic symptoms in daily activities (P = .008) and fewer cognitive symptoms (P = .01).
CONCLUSION: HA-WBRT plus memantine better preserves cognitive function and patient-reported symptoms, with no difference in intracranial PFS and OS, and should be considered a standard of care for patients with good performance status who plan to receive WBRT for brain metastases with no metastases in the HA region.
PMID:32058845 | PMC:PMC7106984 | DOI:10.1200/JCO.19.02767
View details for PubMedID 32058845
-
More
-
Patterns of Failure Observed in the 2-Step Institution Credentialing Process for NRG Oncology/Radiation Therapy Oncology Group 1005 (NCT01349322) and Lessons Learned Practical radiation oncology
Li XA, Moughan J, White JR, Freedman GM, Arthur DW, Galvin J, Xiao Y, McNulty S, Lyons JA, Kavadi VS, Fields MT, Mitchell MP, Anderson BM, Lock MI, Kokeny KE, Bazan JG, Currey AD, Hijal T, Cheston SB, Vicini FA
2020 Jul-Aug;10(4):265-273. doi: 10.1016/j.prro.2019.11.007. Epub 2019 Nov 29.
-
More
PURPOSE: To investigate patterns of failure in institutional credentialing submissions to NRG/RTOG 1005 with the aim of improving the quality and consistency for future breast cancer protocols.
METHODS AND MATERIALS: NRG/RTOG 1005 allowed the submission of 3-dimensional conformal radiation therapy (3DCRT), intensity-modulated radiation therapy (IMRT), and simultaneous integrated boost (SIB) breast plans. Credentialing required institutions to pass a 2-step quality assurance (QA) process: (1) benchmark, requiring institutions to create a plan with no unacceptable deviations and ≤1 acceptable variation among the dose volume (DV) criteria, and (2) rapid review, requiring each institution's first protocol submission to have no unacceptable deviations among the DV criteria or contours. Overall rates, number of resubmissions, and reasons for resubmission were analyzed for each QA step.
RESULTS: In total, 352 institutions participated in benchmark QA and 280 patients enrolled had rapid review QA. Benchmark initial failure rates were similar for 3DCRT (18%), IMRT (17%), and SIB (18%) plans. For 3DCRT and IMRT benchmark plans, ipsilateral lung most frequently failed the DV criteria, and SIB DV failures were seen most frequently for the heart. Rapid review contour initial failures (35%) were due to target rather than organs at risk. For 29% of the rapid review initial failures, the planning target volume boost eval volume was deemed an unacceptable deviation.
CONCLUSIONS: The review of the benchmark and rapid review QA submissions indicates that acceptable variations or unacceptable deviations for the ipsilateral lung and heart dose constraints were the most commonly observed cause of benchmark QA failure, and unacceptable deviations in target contouring, rather than normal structure contouring, were the most common cause of rapid review QA failure. These findings suggest that a rigorous QA process is necessary for high quality and homogeneity in radiation therapy in multi-institutional trials of breast cancer to ensure that the benefits of radiation therapy far outweigh the risks.
PMID:31790823 | PMC:PMC7255922 | DOI:10.1016/j.prro.2019.11.007
View details for PubMedID 31790823
-
More
-
N-Terminomics/TAILS Profiling of Macrophages after Chemical Inhibition of Legumain Biochemistry
Anderson BM, Almeida Nd, Sekhon H, Young D, Dufour A, Edgington-Mitchell LE
2020 Jan 28;59(3):329-340. doi: 10.1021/acs.biochem.9b00821. Epub 2019 Nov 27.
-
More
Legumain (asparaginyl endopeptidase) is the only protease with a preference for cleavage after asparagine residues. Increased legumain activity is a hallmark of inflammation, neurodegenerative diseases, and cancer, and legumain inhibitors have exhibited therapeutic effects in mouse models of these pathologies. Improved knowledge of its substrates and cellular functions is a requisite to further validation of legumain as a drug target. We, therefore, aimed to investigate the effects of legumain inhibition in macrophages using an unbiased and systematic approach. By shotgun proteomics, we identified 16 094 unique peptides in RAW264.7 cells. Among these, 326 unique peptides were upregulated in response to legumain inhibition, while 241 were downregulated. Many of these proteins were associated with mitochondria and metabolism, especially iron metabolism, indicating that legumain may have a previously unknown impact on related processes. Furthermore, we used N-terminomics/TAILS (terminal amine isotopic labeling of substrates) to identify potential substrates of legumain. We identified three new proteins that are cleaved after asparagine residues, which may reflect legumain-dependent cleavage. We confirmed that frataxin, a mitochondrial protein associated with the formation of iron-sulfur clusters, can be cleaved by legumain. This further asserts a potential contribution of legumain to mitochondrial function and iron metabolism. Lastly, we also identified a potential new cleavage site within legumain itself that may give rise to a 25 kDa form of legumain that has previously been observed in multiple cell and tissue types. Collectively, these data shed new light on the potential functions of legumain and will be critical for understanding its contribution to disease.
PMID:31774660 | DOI:10.1021/acs.biochem.9b00821
View details for PubMedID 31774660
-
More
-
Application of a chemical probe to detect neutrophil elastase activation during inflammatory bowel disease Scientific reports
Anderson BM, Poole DP, Aurelio L, Ng GZ, Fleischmann M, Kasperkiewicz P, Morissette C, Drag M, van Driel R, Schmidt BL, Vanner SJ, Bunnett NW, Edgington-Mitchell LE
2019 Sep 16;9(1):13295. doi: 10.1038/s41598-019-49840-4.
-
More
Neutrophil elastase is a serine protease that has been implicated in the pathogenesis of inflammatory bowel disease. Due to post-translational control of its activation and high expression of its inhibitors in the gut, measurements of total expression poorly reflect the pool of active, functional neutrophil elastase. Fluorogenic substrate probes have been used to measure neutrophil elastase activity, though these tools lack specificity and traceability. PK105 is a recently described fluorescent activity-based probe, which binds to neutrophil elastase in an activity-dependent manner. The irreversible nature of this probe allows for accurate identification of its targets in complex protein mixtures. We describe the reactivity profile of PK105b, a new analogue of PK105, against recombinant serine proteases and in tissue extracts from healthy mice and from models of inflammation induced by oral cancer and Legionella pneumophila infection. We apply PK105b to measure neutrophil elastase activation in an acute model of experimental colitis. Neutrophil elastase activity is detected in inflamed, but not healthy, colons. We corroborate this finding in mucosal biopsies from patients with ulcerative colitis. Thus, PK105b facilitates detection of neutrophil elastase activity in tissue lysates, and we have applied it to demonstrate that this protease is unequivocally activated during colitis.
PMID:31527638 | PMC:PMC6746801 | DOI:10.1038/s41598-019-49840-4
View details for PubMedID 31527638
-
More
-
Integrating survivorship care planning in radiation oncology workflow The Journal of community and supportive oncology
Huenerberg KJ, Anderson BM, Tevaarwerk AJ, Neuman HB, Wilke LG, Seaborne LA, Sesto M
2018 Mar-Apr;16(2):e66-e71. doi: 10.12788/jcso.0392.
-
More
Various groups, including the American College of Surgeons' Commission on Cancer and the National Accreditation Program for Breast Centers, are mandating the provision of a survivorship care plan (SCP) to cancer survivors who have completed curative-intent treatment as a requirement for oncology practice accreditation. This article reviews the development of survivorship care, including survivorship care in radiation oncology. Challenges of developing treatment summaries and SCPs and implementing their delivery are explored. Details of the article include how the University of Wisconsin Health radiation oncology department integrated a survivorship visit into the existing radiation oncology workflow. Oncology practices may benefit from the model described here to meet accreditation requirements for SCP delivery to cancer survivors.
PMID:30631797 | PMC:PMC6322695 | DOI:10.12788/jcso.0392
View details for PubMedID 30631797
-
More
-
Indications for and efficacy of postmastectomy radiotherapy for patients with a favorable response to neoadjuvant chemotherapy Cancer
Francis DM, Witt JS, Anderson BM
2019 Feb 1;125(3):332-334. doi: 10.1002/cncr.31785. Epub 2018 Dec 3.
-
Low cardiac and left anterior descending coronary artery dose achieved with left-sided multicatheter interstitial-accelerated partial breast irradiation Brachytherapy
Witt JS, Gao RW, Sudmeier LJ, Rosenberg SA, Francis DM, Wallace CR, Das RK, Anderson BM
2019 Jan-Feb;18(1):50-56. doi: 10.1016/j.brachy.2018.08.014. Epub 2018 Sep 24.
-
More
PURPOSE: Studies have shown that an additional mean dose of 1 Gy to the heart can increase the relative risk of cardiac events. The purpose of this study was to quantify the dose delivered to the heart and left anterior descending artery (LAD) in a series of patients with left-sided breast cancer (BC) or ductal carcinoma in situ treated with multicatheter-accelerated partial breast irradiation (MC-APBI) at a single institution.
METHODS AND MATERIALS: Patients with left-sided BC or ductal carcinoma in situ treated consecutively from 2005 to 2011 with MC-APBI were retrospectively identified. Cardiac and LAD contours were generated for each patient. Cardiac dosimetry and distance to the planning target volume were recorded. Patient health records were reviewed and cardiac events were recorded based on Common Terminology Criteria for Adverse Events version 4.0.
RESULTS: Twenty consecutive patients with left-sided BC treated with MC-APBI were retrospectively identified. Median followup was 41.4 months. Mean equivalent dose in 2 Gy fractions delivered to the heart and LAD were 1.3 (standard deviation: 0.7, range: 0.2-2.9) and 3.8 (standard deviation: 3.0, range: 0.4-11.3) Gy, respectively. There was an inverse linear relationship (R2 = 0.52) between heart-to-lumpectomy cavity distance and mean heart equivalent dose in 2 Gy fractions. One patient (5%) experienced symptomatic cardiac toxicity.
CONCLUSIONS: MC-APBI consistently delivers average doses to the heart and LAD that are similar to those achieved in most series with deep inspiration breath-hold and lower than free-breathing radiotherapy techniques. Distance from the heart to the lumpectomy cavity and the availability of other heart-sparing technologies should be considered to minimize the risk of cardiac toxicity.
PMID:30262411 | PMC:PMC6338487 | DOI:10.1016/j.brachy.2018.08.014
View details for PubMedID 30262411
-
More
-
Results From 10 Years of a Free Oral Cancer Screening Clinic at a Major Academic Health Center International journal of radiation oncology, biology, physics
Blitzer GC, Rosenberg SA, Anderson BM, McCulloch TM, Wieland AM, Hartig GK, Bruce JY, Witek ME, Kimple RJ, Harari PM
2018 Sep 1;102(1):146-148. doi: 10.1016/j.ijrobp.2018.05.007. Epub 2018 Jul 3.
-
More
PMID:29980415 | PMC:PMC6089656 | DOI:10.1016/j.ijrobp.2018.05.007
View details for PubMedID 29980415
-
More
-
Novel use of ViewRay MRI guidance for high-dose-rate brachytherapy in the treatment of cervical cancer Brachytherapy
Ko HC, Huang JY, Miller JR, Das RK, Wallace CR, Costa AD, Francis DM, Straub MR, Anderson BM, Bradley KA
2018 Jul-Aug;17(4):680-688. doi: 10.1016/j.brachy.2018.04.005. Epub 2018 Jun 7.
-
More
PURPOSE: To characterize image quality and feasibility of using ViewRay MRI (VR)-guided brachytherapy planning for cervical cancer.
METHODS AND MATERIALS: Cervical cancer patients receiving intracavitary brachytherapy with tandem and ovoids, planned using 0.35T VR MRI at our institution, were included in this series. The high-risk clinical target volume (HR-CTV), visible gross tumor volume, bladder, sigmoid, bowel, and rectum contours for each fraction of brachytherapy were evaluated for dosimetric parameters. Typically, five brachytherapy treatments were planned using the T2 sequence on diagnostic MRI for the first and third fractions, and a noncontrast true fast imaging with steady-state precession sequence on VR or CT scan for the remaining fractions. Most patients received 5.5 Gy × 5 fractions using high-dose-rate Ir-192 following 45 Gy of whole-pelvis radiotherapy. The plan was initiated at 5.5 Gy to point A and subsequently optimized and prescribed to the HR-CTV. The goal equivalent dose in 2 Gy fractions for the combined external beam and brachytherapy dose was 85 Gy. Soft-tissue visualization using contrast-to-noise ratios to distinguish normal tissues from tumor at their interface was compared between diagnostic MRI, CT, and VR.
RESULTS: One hundred and forty-two fractions of intracavitary brachytherapy were performed from April 2015 to January 2017 on 29 cervical cancer patients, ranging from stages IB1 to IVA. The median HR-CTV was 27.78 cc, with median D90 HR-CTV of 6.1 Gy. The median time from instrument placement to start of treatment using VR was 65 min (scan time 2 min), compared to 105 min using diagnostic MRI (scan time 11 min) (t-test, p < 0.01). The contrast-to-noise ratio of tumor to cervix in both diagnostic MRI and VR had significantly higher values compared to CT (ANOVA and t-tests, p < 0.01).
CONCLUSIONS: We report the first clinical use of VR-guided brachytherapy. Time to treatment using this approach was shorter compared to diagnostic MRI. VR also provided significant advantage in visualizing the tumor and cervix compared to CT. This presents a feasible and reliable manner to image and plan gynecologic brachytherapy.
PMID:29773331 | DOI:10.1016/j.brachy.2018.04.005
View details for PubMedID 29773331
-
More
-
Significant suppression of radiation dermatitis in breast cancer patients using a topically applied adrenergic vasoconstrictor Radiation oncology (London, England)
Cleary JF, Anderson BM, Eickhoff JC, Khuntia D, Fahl WE
2017 Dec 22;12(1):201. doi: 10.1186/s13014-017-0940-7.
-
More
BACKGROUND: Our previous studies showed that vasoconstrictor applied topically to rat skin minutes before irradiation completely prevented radiodermatitis. Here we report on a Phase IIa study of topically applied NG12-1 vasoconstrictor to prevent radiodermatitis in post-lumpectomy breast cancer patients who received at least 40 Gray to the whole breast using standard regimens.
METHODS: Patients had undergone surgery for Stage Ia, Ib, or IIa infiltrating ductal or lobular carcinoma of the breast or ductal carcinoma in situ. NG12-1 formulation was applied topically to the same 50-cm2 treatment site within the radiation field 20 min before each daily radiotherapy fraction.
RESULTS: Scores indicated significant reductions in radiodermatitis at the NG12-1 treatment site versus control areas in the same radiotherapy field. The mean dermatitis score for all subjects was 0.47 (SD 0.24) in the NG12-1-treated area versus 0.72 (SD 0.22) in the control area (P = 0.022). Analysis by two independent investigators indicated radiodermatitis reductions in 9 of the 9 patients with scorable radiodermatitis severity, and one patient with insufficient radiodermatitis to enable scoring. There were no serious adverse events from NG12-1 treatment.
CONCLUSIONS: Thirty, daily, NG12-1 treatments, topically applied minutes before radiotherapy, were well tolerated and conferred statistically significant reductions in radiodermatitis severity (P = 0.022).
TRIAL REGISTRATION: NCT01263366 ; clinicaltrials.gov.
PMID:29273054 | PMC:PMC5741935 | DOI:10.1186/s13014-017-0940-7
View details for PubMedID 29273054
-
More
-
Clinical implementation of a novel Double-Balloon single-entry breast brachytherapy applicator Brachytherapy
Anderson BM, Wallace CR, Costa AD, Das RK
2017 Nov-Dec;16(6):1239-1245. doi: 10.1016/j.brachy.2017.07.015. Epub 2017 Aug 24.
-
More
PURPOSE: The purpose of the study was to describe the clinical utilization of a novel Double-Balloon applicator for accelerated partial breast irradiation (APBI).
METHODS AND MATERIALS: The Double-Balloon single-entry breast applicator contains a single central treatment catheter, as well as four peripheral catheters that can be differentially loaded to customize radiation dose coverage. An inner balloon is filled with up to 7-30 cm3 of saline to increase separation between the peripheral catheters, and an outer balloon is filled with up to 37-115 cm3 of saline to displace breast tissue from the peripheral catheters. Treatment planning objectives include coverage of the breast planning target volume to a minimum of V90 > 90%, limiting dose heterogeneity such that V200 < 10 cm3 and V150 < 50 cm3, and limiting maximum dose to skin (<100% of prescription dose) and ribs (<145% of prescription dose).
RESULTS: High-dose-rate APBI was delivered to 11 women using this device (34 Gy in 10 twice daily fractions). The mean V90 was 98.2% (range 94.2-99.4%). The mean skin Dmax with the Double-Balloon applicator was 83.3% (range 75.6-99.5%). The mean breast V200 was 5.8 cm3 (range 2.3-10.2 cm3), and the mean breast V150 was 32.9 cm3 (range 25.0-41.7 cm3). Pretreatment quality assurance was performed using CT prior to each morning fraction and ultrasound prior to each afternoon fraction.
CONCLUSIONS: The Double-Balloon applicator can be easily introduced into a previously existing brachytherapy program. APBI plans created with this applicator achieve excellent planning target volume coverage, while limiting skin dose and maintaining breast V200 < 10 cm3.
PMID:28844820 | DOI:10.1016/j.brachy.2017.07.015
View details for PubMedID 28844820
-
More
-
MR Imaging of Cervical Cancer Magnetic resonance imaging clinics of North America
Patel-Lippmann K, Robbins JB, Barroilhet L, Anderson B, Sadowski EA, Boyum J
2017 Aug;25(3):635-649. doi: 10.1016/j.mric.2017.03.007. Epub 2017 May 27.
-
More
Cervical cancer is a significant cause of morbidity and mortality worldwide despite advances in screening and prevention. Although cervical cancer remains clinically staged, the 2009 International Federation of Gynecology and Obstetrics committee has encouraged the use of advanced imaging modalities, including MR imaging, where available, to increase the accuracy of staging, guide treatment, and detect recurrence. Understanding the multiple roles of advanced imaging in the evaluation of cervical cancer will help radiologists provide an accurate and useful report to the referring clinicians.
PMID:28668164 | DOI:10.1016/j.mric.2017.03.007
View details for PubMedID 28668164
-
More
-
Locoregional recurrence by molecular subtype after multicatheter interstitial accelerated partial breast irradiation: Results from the Pooled Registry Of Multicatheter Interstitial Sites research group Brachytherapy
Anderson BM, Kamrava M, Wang P, Chen P, Demanes DJ, Hayes JK, Kuske RR
2016 Nov-Dec;15(6):788-795. doi: 10.1016/j.brachy.2016.08.012. Epub 2016 Oct 12.
-
More
PURPOSE: To determine in breast tumor recurrence (IBTR) and regional nodal recurrence (RNR) rates for women treated with multicatheter interstitial accelerated partial breast irradiation.
METHODS AND MATERIALS: Data from five institutions were collected for patients treated from 1992 to 2013. We report outcomes of 582 breast cancers with ≥1 year of followup. Molecular subtype approximation was performed using estrogen receptor, progesterone receptor, Her2, and grade. The Kaplan-Meier method was used to calculate overall survival, IBTR, RNR, and distant recurrence rates. Univariate and multivariate Cox proportional hazard models were performed to estimate risks of IBTR and RNR.
RESULTS: With a median followup time of 5.4 years, the 5-year IBTR rate was 4.7% overall, 3.5% for Luminal A, 4.1% for Luminal B, 5.2% for Luminal Her2, 13.3% for Her2, and 11.3% for triple-negative breast cancer. Positive surgical margins and high grade were associated with increased risk for IBTR, as was Her2 subtype in comparison with Luminal A subtype. Other individual subtypes comparisons did not show a significant difference. Analysis of Luminal A vs. all other subtypes demonstrated lower IBTR risk for Luminal A (5-year IBTR 3.5% vs. 7.3%, p = 0.02). The 5-year RNR rate was 2.1% overall, 0.3% for Luminal A, 4.6% for Luminal B, 2.6% for Luminal Her2, 34.5% for Her2, and 2.3% for triple-negative breast cancer. RNR risk was higher for women with Her2 compared to the other four subtypes and for Luminal B compared to Luminal A subtype.
CONCLUSIONS: Molecular subtype influences IBTR and RNR rates in women treated with multicatheter interstitial accelerated partial breast irradiation.
PMID:27743957 | DOI:10.1016/j.brachy.2016.08.012
View details for PubMedID 27743957
-
More
-
Outcomes of Node-positive Breast Cancer Patients Treated With Accelerated Partial Breast Irradiation Via Multicatheter Interstitial Brachytherapy: The Pooled Registry of Multicatheter Interstitial Sites (PROMIS) Experience American journal of clinical oncology
Kamrava M, Kuske RR, Anderson B, Chen P, Hayes J, Quiet C, Wang P, Veruttipong D, Snyder M, Demanes DJ
2018 Jun;41(6):538-543. doi: 10.1097/COC.0000000000000334.
-
More
OBJECTIVES: To report outcomes for breast-conserving therapy using adjuvant accelerated partial breast irradiation (APBI) with interstitial multicatheter brachytherapy in node-positive compared with node-negative patients.
MATERIALS AND METHODS: From 1992 to 2013, 1351 patients (1369 breast cancers) were treated with breast-conserving surgery and adjuvant APBI using interstitial multicatheter brachytherapy. A total of 907 patients (835 node negative, 59 N1a, and 13 N1mic) had >1 year of data available and nodal status information and are the subject of this analysis. Median age (range) was 59 years old (22 to 90 y). T stage was 90% T1 and ER/PR/Her2 was positive in 87%, 71%, and 7%. Mean number of axillary nodes removed was 12 (SD, 6). Cox multivariate analysis for local/regional control was performed using age, nodal stage, ER/PR/Her2 receptor status, tumor size, grade, margin, and adjuvant chemotherapy/antiestrogen therapy.
RESULTS: The mean (SD) follow-up was 7.5 years (4.6). The 5-year actuarial local control (95% confidence interval) in node-negative versus node-positive patients was 96.3% (94.5-97.5) versus 95.8% (87.6-98.6) (P=0.62). The 5-year actuarial regional control in node-negative versus node-positive patients was 98.5% (97.3-99.2) versus 96.7% (87.4-99.2) (P=0.33). The 5-year actuarial freedom from distant metastasis and cause-specific survival were significantly lower in node-positive versus node-negative patients at 92.3% (82.4-96.7) versus 97.8% (96.3-98.7) (P=0.006) and 91.3% (80.2-96.3) versus 98.7% (97.3-99.3) (P=0.0001). Overall survival was not significantly different. On multivariate analysis age 50 years and below, Her2 positive, positive margin status, and not receiving chemotherapy or antiestrogen therapy were associated with a higher risk of local/regional recurrence.
CONCLUSIONS: Patients who have had an axillary lymph node dissection and limited node-positive disease may be candidates for treatment with APBI. Further research is ultimately needed to better define specific criteria for APBI in node-positive patients.
PMID:27672743 | DOI:10.1097/COC.0000000000000334
View details for PubMedID 27672743
-
More
-
Online patient information from radiation oncology departments is too complex for the general population Practical radiation oncology
Rosenberg SA, Francis DM, Hullet CR, Morris ZS, Brower JV, Anderson BM, Bradley KA, Bassetti MF, Kimple RJ
2017 Jan-Feb;7(1):57-62. doi: 10.1016/j.prro.2016.07.008. Epub 2016 Aug 1.
-
More
PURPOSE: Nearly two-thirds of cancer patients seek information about their diagnosis online. We assessed the readability of online patient education materials found on academic radiation oncology department Web sites to determine whether they adhered to guidelines suggesting that information be presented at a sixth-grade reading level.
METHODS AND MATERIALS: The Association of American Medical Colleges Web site was used to identify all academic radiation oncology departments in the United States. One-third of these department Web sites were selected for analysis using a random number generator. Both general information on radiation therapy and specific information regarding various radiation modalities were collected. To test the hypothesis that the readability of these online educational materials was written at the recommended grade level, a panel of 10 common readability tests was used. A composite grade level of readability was constructed using the 8 readability measures that provide a single grade-level output.
RESULTS: A mean of 5605 words (range, 2058-12,837) from 30 department Web sites was collected. Using the composite grade level score, the overall mean readability level was determined to be 13.36 (12.83-13.89), corresponding to a collegiate reading level. This was significantly higher than the target sixth-grade reading level (middle school, t (29) = 27.41, P < .001).
CONCLUSIONS: Online patient educational materials from academic radiation oncology Web sites are significantly more complex than recommended by the National Institutes of Health and the Department of Health and Human Services. To improve patients' comprehension of radiation therapy and its role in their treatment, our analysis suggests that the language used in online patient information should be simplified to communicate the information at a more appropriate level.
PMID:27663932 | PMC:PMC5219938 | DOI:10.1016/j.prro.2016.07.008
View details for PubMedID 27663932
-
More
-
Readability of Online Patient Educational Resources Found on NCI-Designated Cancer Center Web Sites Journal of the National Comprehensive Cancer Network : JNCCN
Rosenberg SA, Francis D, Hullett CR, Morris ZS, Fisher MM, Brower JV, Bradley KA, Anderson BM, Bassetti MF, Kimple RJ
2016 Jun;14(6):735-40. doi: 10.6004/jnccn.2016.0075.
-
More
BACKGROUND: The NIH and Department of Health & Human Services recommend online patient information (OPI) be written at a sixth grade level. We used a panel of readability analyses to assess OPI from NCI-Designated Cancer Center (NCIDCC) Web sites.
METHODS: Cancer.gov was used to identify 68 NCIDCC Web sites from which we collected both general OPI and OPI specific to breast, prostate, lung, and colon cancers. This text was analyzed by 10 commonly used readability tests: the New Dale-Chall Readability Formula, Flesch Reading Ease scale, Flesch-Kinaid Grade Level, FORCAST scale, Fry Readability Graph, Simple Measure of Gobbledygook test, Gunning Frequency of Gobbledygook index, New Fog Count, Raygor Readability Estimate Graph, and Coleman-Liau Index. We tested the hypothesis that the readability of NCIDCC OPI was written at the sixth grade level. Secondary analyses were performed to compare readability of OPI between comprehensive and noncomprehensive centers, by region, and to OPI produced by the American Cancer Society (ACS).
RESULTS: A mean of 30,507 words from 40 comprehensive and 18 noncomprehensive NCIDCCs was analyzed (7 nonclinical and 3 without appropriate OPI were excluded). Using a composite grade level score, the mean readability score of 12.46 (ie, college level: 95% CI, 12.13-12.79) was significantly greater than the target grade level of 6 (middle-school: P<.001). No difference between comprehensive and noncomprehensive centers was identified. Regional differences were identified in 4 of the 10 readability metrics (P<.05). ACS OPI provides easier language, at the seventh to ninth grade level, across all tests (P<.01).
CONCLUSIONS: OPI from NCIDCC Web sites is more complex than recommended for the average patient.
PMID:27283166 | PMC:PMC7236813 | DOI:10.6004/jnccn.2016.0075
View details for PubMedID 27283166
-
More
-
Pitfalls in Imaging of Cervical Cancer Seminars in roentgenology
Robbins J, Kusmirek J, Barroilhet L, Anderson B, Bradley K, Sadowski E
2016 Jan;51(1):17-31. doi: 10.1053/j.ro.2015.11.001. Epub 2015 Nov 26.
-
Temporal Trends in Postmastectomy Radiation Therapy and Breast Reconstruction Associated With Changes in National Comprehensive Cancer Network Guidelines JAMA oncology
Frasier LL, Holden S, Holden T, Schumacher JR, Leverson G, Anderson B, Greenberg CC, Neuman HB
2016 Jan;2(1):95-101. doi: 10.1001/jamaoncol.2015.3717.
-
More
IMPORTANCE: Evolving data on the effectiveness of postmastectomy radiation therapy (PMRT) have led to changes in National Comprehensive Cancer Network (NCCN) recommendations, counseling clinicians to "strongly consider" PMRT for patients with breast cancer with tumors 5 cm or smaller and 1 to 3 positive nodes; however, anticipation of PMRT may lead to delay or omission of reconstruction, which can have cosmetic, quality-of-life, and complication implications for patients.
OBJECTIVE: To determine whether revised guidelines have increased PMRT and affected receipt of breast reconstruction. We hypothesized that (1) PMRT rates would increase for women affected by the revised guidelines while remaining stable in other cohorts and (2) receipt of breast reconstruction would decrease in these women while increasing in other groups.
DESIGN, SETTING, AND PARTICIPANTS: Retrospective, population-based cohort study of Surveillance, Epidemiology, and End Results (SEER) data on women with stage I to III breast cancer undergoing mastectomy from 2000 through 2011. Our analytic sample (N = 62,442) was divided into cohorts on the basis of current NCCN radiotherapy recommendations: "radiotherapy recommended" (tumors > 5 cm or ≥ 4 positive lymph nodes), "strongly consider radiotherapy" (tumor ≤ 5 cm, 1-3 positive nodes), and "radiotherapy not recommended" (tumors ≤ 5 cm, no positive nodes).
MAIN OUTCOMES AND MEASURES: We used Joinpoint regression analysis to evaluate temporal trends in receipt of PMRT and breast reconstruction.
RESULTS: The 3 cohorts comprised 15,999 in the "radiotherapy recommended" group, 15,006 in the "strongly consider radiotherapy" group, and 31,837 in the "radiotherapy not recommended" group. [corrected]. Rates of PMRT were unchanged in the radiotherapy recommended (29.9%) and radiotherapy not recommended (7.4%) cohorts over the study period. Receipt of PMRT for the strongly consider radiotherapy cohort was unchanged at 26.9% until 2007. At that time, a significant change in the APC was observed (P = .01) with an increase in APC from 2.1% to 9.0% (P = .02) through the end of the study period, for a final rate of 40.5%. Breast reconstruction increased across all cohorts. Despite increasing receipt of PMRT, the strongly consider radiotherapy cohort maintained a consistent increase in reconstruction (annual percentage change, 7.4%) throughout the study period. This is similar to the increase in reconstruction observed for the radiotherapy recommended (10.7%) and radiotherapy not recommended (8.4%) cohorts.
CONCLUSIONS AND RELEVANCE: Changes in NCCN guidelines have been associated with an increase in PMRT among patients with tumors 5 cm or smaller and 1 to 3 positive nodes without an associated decrease in receipt of reconstruction. This may represent increasing clinician comfort with irradiating a new breast reconstruction and may have cosmetic and quality-of-life implications for patients.
PMID:26539936 | PMC:PMC4713236 | DOI:10.1001/jamaoncol.2015.3717
View details for PubMedID 26539936
-
More
-
Oncologists' Perspectives of Their Roles and Responsibilities During Multi-disciplinary Breast Cancer Follow-Up Annals of surgical oncology
Neuman HB, Steffens NM, Jacobson N, Tevaarwerk A, Anderson B, Wilke LG, Greenberg CC
2016 Mar;23(3):708-14. doi: 10.1245/s10434-015-4904-6. Epub 2015 Oct 16.
-
More
BACKGROUND: Improving the quality of follow-up provided to the 3 million U.S. breast cancer survivors is a high priority. Current guidelines do not provide guidance regarding who should participate in follow-up or what providers' specific responsibilities should be. Given the multidisciplinary nature of breast cancer care, this results in significant variation and creates the potential for redundancy and/or gaps. Our objective was to provide insight into why different types of oncologists believe their participation in follow-up is necessary.
METHODS: A purposeful sample of breast medical, radiation, and surgical oncologists was identified (n = 35) and in-depth one-on-one interviews were conducted. Data were analyzed using content analysis.
RESULTS: Medical oncologists were driven by a sense of Responsibility for Ongoing Therapy, perceived Strong Patient Relationship, and belief that their systemic approach to follow-up represented a Specific Skillset beneficial to patients. In contrast, surgical and radiation oncologists were selective about which patients they followed, participating when they perceived their Specific Skillset of enhanced local-regional assessments would be valuable. Additionally, they endorsed participating to Ensure Follow-up is Received or not participating to Minimize Redundancy. These individual decisions led to either a Complementary Oncologist Team or Primary Oncologist follow-up approach.
CONCLUSIONS: Oncologists' feel responsible for the cancer-related components of follow-up. Differences amongst oncology specialists' perceived responsibilities influenced decisions to provide ongoing follow-up. Based on these individual decisions, a Complementary Oncologist Team or Primary Oncologist model of care evolves organically. Guidelines that explicitly direct patients into a care model have the potential to significantly improve care quality and efficiency.
PMID:26474556 | PMC:PMC4749446 | DOI:10.1245/s10434-015-4904-6
View details for PubMedID 26474556
-
More
-
Outcomes of Breast Cancer Patients Treated with Accelerated Partial Breast Irradiation Via Multicatheter Interstitial Brachytherapy: The Pooled Registry of Multicatheter Interstitial Sites (PROMIS) Experience Annals of surgical oncology
Kamrava M, Kuske RR, Anderson B, Chen P, Hayes J, Quiet C, Wang P, Veruttipong D, Snyder M, Demanes DJ
2015 Dec;22 Suppl 3:S404-11. doi: 10.1245/s10434-015-4563-7. Epub 2015 Apr 28.
-
More
PURPOSE: To report outcomes for breast-conserving therapy using adjuvant accelerated partial breast irradiation with interstitial multicatheter brachytherapy by a cooperative group of institutions.
METHODS: From 1992 to 2013, a total of 1356 patients were treated with breast-conserving surgery and adjuvant accelerated partial breast irradiation using interstitial multicatheter brachytherapy. A total of 1131 patients had >1 year of data available to assess oncologic and cosmesis outcomes. Median age was 59 years old (range 22-90 years). Histologies treated included 1005 (73 %) invasive ductal carcinoma and 240 (18 %) ductal carcinoma-in situ. T stages were 18 % Tis, 75 % T1, and 8 % ≥T2. Nodal status was 73 % N0 and 6 % N1a. Estrogen receptor, progesterone receptor, and human epidermal growth factor receptor 2 was positive in 83, 70, and 6 %, respectively. Cox multivariate analysis for local control was performed using histology, age, estrogen receptor status, tumor size, grade, margin, and nodal status.
RESULTS: The mean (SD) follow-up was 6.9 years (4.3). The 10-year actuarial risk (95 % confidence interval) of an ipsilateral breast tumor recurrence was 7.6 % (5.6-10.1). Other 10-year actuarial risks (95 % confidence interval) were regional failure 2.3 % (1.4-3.7), distant metastasis 3.8 % (2.5-5.7), cause-specific survival 96.3 % (94.2-97.6), overall survival 86.5 (83.0-89.3), and new contralateral cancers 4.6 % (3.0-6.9). On multivariate analysis, high grade (hazard ratio 2.81) and positive margin status (hazard ratio 18.42) were the only two significant variables associated with an increased risk of local recurrence. Physician-reported cosmesis was excellent/good in 84 % (98 of 116) of patients with >5 years of follow-up.
CONCLUSIONS: This is the largest report of outcomes with interstitial breast brachytherapy. This treatment resulted in excellent long-term local control and cosmesis outcomes.
PMID:25916980 | DOI:10.1245/s10434-015-4563-7
View details for PubMedID 25916980
-
More
-
PET/CT and MRI in the imaging assessment of cervical cancer Abdominal imaging
Kusmirek J, Robbins J, Allen H, Barroilhet L, Anderson B, Sadowski EA
2015 Oct;40(7):2486-511. doi: 10.1007/s00261-015-0363-6.
-
More
Imaging plays a central role in the evaluation of patients with cervical cancer and helps guide treatment decisions. The purpose of this pictorial review is to describe magnetic resonance (MR) imaging and positron emission tomography (PET)/computed tomography (CT) assessment of cervical cancer, including indications for imaging, important findings that may result in management change, as well as limitations of both modalities. The International Federation of Gynecology and Obstetrics cervical cancer staging system does not officially include imaging; however, the organization endorses the use of MR imaging and PET/CT in the management of patients with cervical cancer where these modalities are available. MR imaging provides the best visualization of the primary tumor and extent of soft tissue disease. PET/CT is recommended for assessment of nodal involvement, as well as distant metastases. Both MR imaging and PET/CT are used to follow patients post-treatment to assess for recurrence. This review focuses on the current MR imaging and PET/CT protocols, the utility of these modalities in assessing primary tumors and recurrences, with emphasis on imaging findings which change management and on imaging pitfalls to avoid. It is important to be familiar with the MR imaging and PET/CT appearance of the primary tumor and metastasis, as well as the imaging pitfalls, so that an accurate assessment of disease burden is made prior to treatment.
PMID:25666968 | DOI:10.1007/s00261-015-0363-6
View details for PubMedID 25666968
-
More
-
Impact of adjuvant pelvic radiotherapy in stage I uterine sarcoma Anticancer research
Magnuson WJ, Petereit DG, Anderson BM, Geye HM, Bradley KA
2015 Jan;35(1):365-70.
-
More
BACKGROUND/AIM: The optimal adjuvant therapy for stage I uterine sarcoma remains unresolved and may consist of radiotherapy (RT), chemotherapy, hormonal therapy or observation. We analyzed the impact of adjuvant pelvic RT on overall survival (OS), cause-specific survival (CSS), disease-free survival (DFS), pelvic control (PC) and patterns of failure.
PATIENTS AND METHODS: A retrospective analysis of 157 patients with International Federation of Gynecology and Obstetrics FIGO stage I uterine sarcoma was performed. RT was given postoperatively to a dose of 45-51 Gy in 28-30 fractions.
RESULTS: The 5-year OS, CSS, DFS and PC was 58%, 62%, 47% and 72%, respectively. Adjuvant RT significantly improved PC (85% for RT group vs. 64% for non-RT group; p=0.02) but did not impact OS, CSS or DFS.
CONCLUSION: The addition of adjuvant pelvic RT significantly improved PC for patients with stage I uterine sarcoma. As systemic therapies continue to improve, optimal locoregional control may result in improved patient outcomes.
PMID:25550573
View details for PubMedID 25550573
-
More
-
Upper abdominal normal organ contouring guidelines and atlas: a Radiation Therapy Oncology Group consensus Practical radiation oncology
Jabbour SK, Hashem SA, Bosch W, Kim TK, Finkelstein SE, Anderson BM, Ben-Josef E, Crane CH, Goodman KA, Haddock MG, Herman JM, Hong TS, Kachnic LA, Mamon HJ, Pantarotto JR, Dawson LA
2014 Mar-Apr;4(2):82-89. doi: 10.1016/j.prro.2013.06.004. Epub 2013 Aug 7.
-
More
PURPOSE: To standardize upper abdominal normal organ contouring guidelines for Radiation Therapy Oncology Group (RTOG) trials.
METHODS AND MATERIALS: Twelve expert radiation oncologists contoured the liver, esophagus, gastroesophageal junction (GEJ), stomach, duodenum, and common bile duct (CBD), and reviewed and edited 33 additional normal organ and blood vessel contours on an anonymized patient computed tomography (CT) dataset. Contours were overlaid and compared for agreement using MATLAB (MathWorks, Natick, MA). S95 contours, defined as the binomial distribution to generate 95% group consensus contours, and normal organ contouring definitions were generated and reviewed by the panel.
RESULTS: There was excellent consistency and agreement of the liver, duodenal, and stomach contours, with substantial consistency for the esophagus contour, and moderate consistency for the GEJ and CBD contours using a Kappa statistic. Consensus definitions, detailed normal organ contouring recommendations and high-resolution images were developed.
CONCLUSIONS: Consensus contouring guidelines and a CT image atlas should improve contouring uniformity in radiation oncology clinical planning and RTOG trials.
PMID:24890348 | PMC:PMC4285338 | DOI:10.1016/j.prro.2013.06.004
View details for PubMedID 24890348
-
More
-
Predictive factors of recurrence following adjuvant vaginal cuff brachytherapy alone for stage I endometrial cancer Gynecologic oncology
Dunn EF, Geye H, Platta CS, Gondi V, Rose S, Bradley KA, Anderson BM
2014 Jun;133(3):494-8. doi: 10.1016/j.ygyno.2014.03.554. Epub 2014 Mar 20.
-
More
PURPOSE: The purpose of this study is to identify risk factors for recurrence in a cohort of stage I endometrial cancer patients treated with vaginal cuff brachytherapy at a single academic institution.
METHODS AND MATERIALS: From 1989 to 2011, 424 patients with stage I endometrial cancer underwent total hysterectomy and bilateral salpingo-oophorectomy, with or without lymphadenectomy (LND), followed by high-dose-rate vaginal cuff brachytherapy (VCB) to patients felt to be high or intermediate risk FIGO stage IA and IB disease. Covariates included: 2009 FIGO stage, age, grade, histology, presence of lymphovascular space invasion, LND, and receipt of chemotherapy.
RESULTS: With a median follow-up of 3.7years, the 5 and 10-year disease free survival were 98.4% and 95.9%, respectively. A total of 30 patients developed recurrence, with the predominant pattern of isolated distant recurrence (57.0%). On multivariate analysis, grade 3 (p=0.039) and LND (p=0.048) independently predicted of increased recurrence risk. χ(2) analysis suggested that higher-risk patients were selected for LND, with significant differences in age, stage, and grade noted between cohorts. Distant metastatic rate was significantly higher for patients who qualified for GOG 0249 at 23.1% (95% CI 10.7-35.5%) compared to those who did not at 6.8% (95% CI 1.8-11.8%, p<0.001).
CONCLUSION: Overall disease-free survival for this cohort of patients was >95% at 10years. Univariate analysis confirmed previously identified risk factors as predictors for recurrence. Multivariate analysis found that grade 3 and LND correlated with risk for recurrence. Of those that did recur, the initial site of relapse included distant metastasis in most cases.
PMID:24657301 | DOI:10.1016/j.ygyno.2014.03.554
View details for PubMedID 24657301
-
More
-
Single institution experience treating 104 vestibular schwannomas with fractionated stereotactic radiation therapy or stereotactic radiosurgery Journal of neuro-oncology
Anderson BM, Khuntia D, Bentzen SM, Geye HM, Hayes LL, Kuo JS, Baskaya MK, Badie B, Basavatia A, Pyle GM, Tomé WA, Mehta MP
2014 Jan;116(1):187-93. doi: 10.1007/s11060-013-1282-4. Epub 2013 Oct 20.
-
More
The pupose of this study is to assess the long-term outcome and toxicity of fractionated stereotactic radiation therapy (FSRT) and stereotactic radiosurgery (SRS) for 100 vestibular schwannomas treated at a single institution. From 1993 to 2007, 104 patients underwent were treated with radiation therapy for vestibular schwannoma. Forty-eight patients received SRS, with a median prescription dose of 12.5 Gy for SRS (range 9.7-16 Gy). For FSRT, two different fraction schedules were employed: a conventional schedule (ConFSRT) of 1.8 Gy per fraction (Gy/F) for 25 or 28 fractions to a total dose of 45 or 50.4 Gy (n = 19); and a once weekly hypofractionated course (HypoFSRT) consisting of 4 Gy/F for 5 fractions to a total dose of 20 Gy (n = 37). Patients treated with FSRT had better baseline hearing, facial, and trigeminal nerve function, and were more likely to have a diagnosis of NF2. The 5-year progression free rate (PFR) was 97.0 after SRS, 90.5% after HypoFSRT, and 100.0% after ConFSRT (p = NS). Univariate analysis demonstrated that NF2 and larger tumor size (greater than the median) correlated with poorer local control, but prior surgical resection did not. Serviceable hearing was preserved in 60.0% of SRS patients, 63.2% of HypoFSRT patients, and 44.4% of ConFSRT patients (p = 0.6). Similarly, there were no significant differences in 5-year rates of trigeminal toxicity facial nerve toxicity, vestibular dysfunction, or tinnitus.
CONCLUSIONS: Equivalent 5-year PFR and toxicity rates are shown for patients with vestibular schwanoma selected for SRS, HypoFSRT, and ConFSRT after multidisciplinary evaluation. Factors correlating with tumor progression included NF2 and larger tumor size.
PMID:24142200 | DOI:10.1007/s11060-013-1282-4
View details for PubMedID 24142200
-
More
-
Adjuvant and definitive radiation therapy for primary carcinoma of the vagina using brachytherapy and external beam radiation therapy Journal of contemporary brachytherapy
Platta CS, Anderson B, Geye H, Das R, Straub M, Bradley K
2013 Jun;5(2):76-82. doi: 10.5114/jcb.2013.36177. Epub 2013 Jun 28.
-
More
PURPOSE: To report the outcomes of patients receiving vaginal brachytherapy and/or external beam radiation therapy (EBRT) for primary vaginal cancer.
MATERIAL AND METHODS: Between 1983 and 2009, 63 patients received brachytherapy and/or EBRT for primary tumors of the vagina at a single tertiary center. Patient data was collected via chart review. The Kaplan-Meier method was used to calculate actuarial pelvic local control (LC), disease-free survival (DFS), overall survival (OS), and severe late toxicity rates. Acute and late toxicities were scored according to the Common Terminology Criteria for Adverse Events version 3 (CTCAE v3.0).
RESULTS: Median follow up was 44.2 months. Patients with early stage disease (stages I and II) had significantly improved 5-year OS when compared to patients with locally advanced disease (stages III and IVA) (73.3 vs. 34.4%, p = 0.032). Patients with greater than 1/3 vaginal involvement had significantly worse prognosis than patients with tumors involving 1/3 or less of the vagina, with the later having superior DFS (84.0 vs. 52.4%, p = 0.007) and LC (86.9 vs. 60.4%, p = 0.018) at 5-years. Age, histology, and brachytherapy technique did not impact treatment outcomes. The 5-year actuarial grade 3 or higher toxicity rate was 23.1% (95% CI: 10.6-35.6%). Concurrent chemotherapy had no impact on outcomes or toxicity in this analysis.
CONCLUSIONS: Success of treatment for vaginal cancer depends primarily on disease stage, but other contributing factors such as extent of vaginal involvement and tumor location significantly impact outcomes. Treatment of vaginal cancer with primary radiotherapy yields acceptable results with reasonable toxicity rates. Management of this rare malignancy requires a multidisciplinary approach to appropriately optimize therapy.
PMID:23878551 | PMC:PMC3708150 | DOI:10.5114/jcb.2013.36177
View details for PubMedID 23878551
-
More
-
Locoregional recurrence following accelerated partial breast irradiation for early-stage invasive breast cancer: significance of estrogen receptor status and other pathological variables Annals of surgical oncology
Cannon DM, McHaffie DR, Patel RR, Adkison JB, Das RK, Anderson BD, Geye HM, Bentzen SM, Cannon GM
2013 Oct;20(11):3446-52. doi: 10.1245/s10434-013-3015-5. Epub 2013 May 25.
-
More
BACKGROUND: Understanding risk factors for locoregional recurrence (LRR) after accelerated partial breast irradiation (APBI) can help to guide patient selection for treatment with APBI. Published findings to date have not been consistent. More data are needed as these risk factors continue to be defined.
METHODS: A total of 277 women with early-stage invasive breast cancer underwent lumpectomy and were treated adjuvantly at our institution with APBI using high-dose rate brachytherapy. APBI was delivered using multicatheter interstitial brachytherapy (91 %) or single-entry catheter brachytherapy (9 %) to a dose of 32-34 Gy in 8-10 twice daily fractions. Failure patterns and risk factors for recurrence were analyzed.
RESULTS: With a median follow-up of 61 months, the 5-year locoregional control rate was 94.4 %. Negative estrogen receptor (ER) status was strongly associated with LRR on multivariate analysis (p < 0.005). Lobular histology, the presence of an extensive intraductal component, and lymphovascular invasion also were significant but to a lesser degree than ER-negative status. Patients with multiple risk factors were at highest risk for LRR. Age was not significantly associated with increased risk for LRR.
CONCLUSIONS: The presence of specific pathological features, particularly ER negative status, was associated with increased risk of LRR in this cohort of women treated with APBI. Further investigation is warranted to determine whether patients with adverse pathological risk factors are at higher risk of LRR after APBI than after conventional whole breast irradiation (WBI), as these same features also may place women at risk for LRR after WBI.
PMID:23709055 | DOI:10.1245/s10434-013-3015-5
View details for PubMedID 23709055
-
More
-
Breast radiation correlates with side of parathyroid adenoma World journal of surgery
Woll ML, Mazeh H, Anderson BM, Chen H, Sippel RS
2012 Mar;36(3):607-11. doi: 10.1007/s00268-011-1394-y.
-
More
BACKGROUND: Prior head and neck irradiation is a known risk factor for hyperparathyroidism. It is not clear whether irradiation for breast cancer, which may expose the neck to radiation, is also a risk factor for hyperparathyroidism. The present study analyzes the association between the side of radiation to the chest following breast surgery and the side of subsequent parathyroid adenoma development.
METHODS: We analyzed a prospective database of 1,428 consecutive patients who underwent parathyroidectomy at our institution between November 2000 and August 2010. Patients who had previously undergone breast surgery were identified. Patients with multigland disease were excluded. Patients with bilateral breast surgery were counted as having had two separate procedures; one on each side. Patients who had radiation therapy following breast surgery (RadRx) were compared to those who had breast surgery without radiation treatment (No RadRx).
RESULTS: A total of 146 breast procedures were performed in 121 patients. Forty procedures were in the RadRx group versus 106 cases in the No RadRx group. Patients with radiation therapy were older (68 ± 1.8 years versus 63 ± 1.2 years; P = 0.02) and had higher preoperative calcium levels (11.3 ± 0.1 mg/dl versus 10.9 ± 0.1 mg/dl; P = 0.001). However, there was no significant difference in either parathyroid hormone (PTH) level or gland weight. The latency period between breast irradiation and parathyroid surgery was 8 ± 0.9 years. Interestingly, the side of radiation therapy was associated with the side of the parathyroid adenoma in 76% of cases, compared to only 44% in those who had breast surgery without radiation exposure (P = 0.0004).
CONCLUSIONS: The present study demonstrates that, similar to prior head and neck radiation, prior breast irradiation correlates with the development of parathyroid disease. Specifically, there is a strong correlation between the side of the radiation therapy and the side of a subsequent parathyroid adenoma. Breast irradiation should therefore be considered a risk factor for the development of parathyroid adenomas.
PMID:22207495 | DOI:10.1007/s00268-011-1394-y
View details for PubMedID 22207495
-
More
-
Current state of knowledge regarding the use of antiangiogenic agents with radiation therapy Cancer treatment reviews
Mazeron R, Anderson B, Supiot S, Paris F, Deutsch E
2011 Oct;37(6):476-86. doi: 10.1016/j.ctrv.2011.03.004. Epub 2011 May 4.
-
More
Angiogenesis has been a central theme of oncologic research for several years. Recently, improved understanding of its mechanisms has led to the development of several antiangiogenic agents. Some have demonstrated their effectiveness in large randomized studies; however, no antiangiogenic agent has yet been approved for treatment in combination with radiotherapy. Numerous preclinical studies and a few small clinical trials have recently reported encouraging results. The objective of this article is to review the concept of targeted antiangiogenic agents and the early clinical results of their use in combination with radiation therapy.
PMID:21546163 | DOI:10.1016/j.ctrv.2011.03.004
View details for PubMedID 21546163
-
More
-
The impact of hybrid PET-CT scan on overall oncologic management, with a focus on radiotherapy planning: a prospective, blinded study Technology in cancer research & treatment
Kruser TJ, Bradley KA, Bentzen SM, Anderson BM, Gondi V, Khuntia D, Perlman SB, Tome WA, Chappell RJ, Walker WL, Mehta MP
2009 Apr;8(2):149-58. doi: 10.1177/153303460900800208.
-
More
Functional imaging using fluorodeoxyglucose positron-emission tomography (FDG-PET) has been increasing incorporated into radiotherapy planning in conjunction with computed tomography (CT). Hybrid FDG-PET/CT scanners allow these images to be obtained in very close temporal proximity without the need for repositioning patients, thereby minimizing imprecision when overlying these images. To prospectively examine the impact of hybrid PET/CT imaging on overall oncologic impact, with a focus on radiotherapy planning, we performed a prospective, blinded trial in 111 patients. Patients with lung cancer (n=38), head-and-neck squamous cell carcinoma (n=23), breast (n=8), cervix (n=15), esophageal (n=9), and lymphoma (n=18) underwent hybrid PET/CT imaging at the time of radiation therapy planning. A physician blinded to the PET dataset designed a treatment plan using all clinical information and the CT dataset. The treating physician subsequently designed a second treatment plan using the hybrid PET/CT dataset. The two treatment plans were compared to determine if a major alteration in overall oncologic management occured. In patients receiving potentially curative radiotherapy the concordance between CT-based and PET/CT-based GTVs was quantified using an index of conformality (CI). In 76/111 (68%) of patients, the PET/CT data resulted in a change in one or more of the following: GTV volume, regional/local extension, prescribed dose, or treatment modality selection. In 35 of these 76 cases (46%; 31.5% of the entire cohort) the change resulted in a major alteration in the oncologic management (dose, field design, or modality change). Thus, nearly a third of all cases had a major alteration in oncologic management as a result of the PET/CT data, and 29 of 105 patients (27.6%) who underwent potentially curative radiotherapy had major alterations in either dose or field design. Hybrid PET/CT imaging at the time of treatment planning may be highly informative and an economical manner in which to obtain PET imaging, with the dual goals of staging and treatment planning.
PMID:19334796 | DOI:10.1177/153303460900800208
View details for PubMedID 19334796
-
More
Contact Information
Bethany Anderson, MD
600 Highland Avenue,Box 3684 Clinical Science Center
Madison, WI 53792
