I am a professor in the Department of Human Oncology. In my clinical practice, I specialize in treating patients with gynecologic, hematologic and pediatric malignancies. I have a very busy brachytherapy practice. I work closely with gynecologic oncologists, hematologists, pediatric oncologists, radiologists and other specialists to best meet my individual patients’ needs.
In addition to my clinical practice, I am the Radiation Oncology Residency Program director. I also am involved with teaching medical students and undergraduates. Fellows from gynecologic oncology and pediatric oncology work with me on clinical rotations yearly.
I perform clinical research, primarily in the area of gynecologic radiation oncology, but I also have served as the principal investigator for a Children’s Oncology Group study on pediatric pontine gliomas.
Dr. Bradley's UW Health ProfileEducation
Residency, University of Wisconsin–Madison, Radiation Oncology (2004)
Transitional Year Intern, St. Luke’s Medical Center, Milwaukee, (2000)
MD, University of Wisconsin–Madison, Medicine (1999)
BS, University of Wisconsin–Madison, Molecular Biology (1994)
Academic Appointments
Professor (CHS), Human Oncology (2019)
Associate Professor (CHS), Human Oncology (2010)
Assistant Professor (CHS), Human Oncology (2004)
Selected Honors and Awards
Madison Magazine Top Doctors (multiple years)
UW Health Patient Experience Physician Champion Award (2016)
UW Health Clinical Practice Excellence Award (2015)
Teacher of the Year Award, The Association of Residents in Radiation Oncology (2007)
Chief Resident, Radiation Oncology, University of Wisconsin (2004)
National Institutes of Health (NIH) Physician-Scientist Training Grant (2002–2003)
Medical School Class Co-President (1995–1996)
Medical Scholars Program, University of Wisconsin (1991–1994)
University of Wisconsin Full Academic Scholarship (1991–1994)
Boards, Advisory Committees and Professional Organizations
American Society for Therapeutic Radiology and Oncology (ASTRO) (2000–pres.)
American Society for Clinical Oncology (ASCO) (2000–pres.)
Children’s Oncology Group (2004–pres.)
American Brachytherapy Society (2006–pres.)
Central Nervous System Tumor Committee, Children’s Oncology Group (COG) (2006–pres.)
Radiation Oncology Committee, Children’s Oncology Group (COG) (2006–pres.)
Scientific Committee and Abstract Reviewer, Gynecologic Section, for Annual Meeting, American Society for Therapeutic Radiology and Oncology (ASTRO) (2008–pres.)
Radiological Society of North America (RSNA) (2007–pres.)
Member, National Comprehensive Cancer Network (NCCN) Cervical, Vulvar, and Uterine Cancers Panel (2016–pres.)
Scientific Program Committee, Annual Meeting of the American Brachytherapy Society (ABS) (2016–2017)
President, Wisconsin Society of Radiation Oncology (2010–2013)
Radiation Oncology Committee, Gynecologic Oncology Group (GOG) (2006–2012)
Item Writing Committee, Gynecologic Section, American Board of Radiology (ABR) – writing questions for use in future ABR Radiation Oncology board certification exams (2007–2012)
Scientific Committee and Abstract Reviewer, Radiation Oncology and Radiobiology Subcommittee, for Annual Meeting, Radiological Society of North America (RSNA) (2007–2012)
Vice President, Wisconsin Society of Radiation Oncology (2008–2010)
Secretary, Wisconsin Society of Radiation Oncology (2007–2008)
International Working Group for Image-Guided Gynecologic Brachytherapy (2006–2008)
Research Focus
Gynecologic Cancer, Hematologic Malignancies, Pediatric Malignancies
Dr. Kristin Bradley specializes in treating patients with gynecologic, hematologic and pediatric malignancies. She has a busy brachytherapy practice and works closely with gynecologic oncologists, hematologists, pediatric oncologists, radiologists and other specialists to best meet her patients’ needs. She also is the Radiation Oncology Residency Program director.
I participate in clinical research, evaluating ways to improve cancer care in patients with gynecologic, hematologic or pediatric cancers who are receiving radiation as a component of their treatment.
Novel Use of 0.35T ViewRay MRI-guidance for High Dose Rate Brachytherapy in the Treatment of Cervical Cancer
Image-guided adaptive brachytherapy for cervical cancer has resulted in improved outcomes and/or decreased toxicity rates for many cervical patients compared to prior 2D/fluoroscopic-based planning. We sought to evaluate the 0.35T MRI on our ViewRay system for brachytherapy and to compare dosimetry, time to treatment and image quality relative to diagnostic MRI and CT.
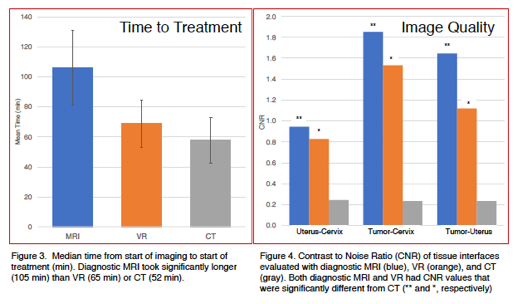
We presented our findings in abstract form at ASTRO 2017 and manuscript has been submitted.
Severe Late Toxicities Following Concomitant Chemoradiotherapy Compared to Radiotherapy Alone in Cervical Cancer: An Inter-Era Analysis
We sought to compare rates of severe late toxicities following concomitant chemoradiotherapy and radiotherapy alone for cervical cancer. We found that compared to radiotherapy alone, concomitant chemoradiotherapy is associated with higher rates of severe vaginal and skeletal late toxicities.
Locations
University Hospitals and Clinics
I am the Radiation Oncology Residency Program director. I also am involved with teaching medical students and undergraduates. Fellows from gynecologic oncology and pediatric oncology work with me on clinical rotations yearly.
Radiation Oncology Residency Page
-
NCCN Guidelines® Insights: Cervical Cancer, Version 1.2024 Journal of the National Comprehensive Cancer Network : JNCCN
Abu-Rustum NR, Yashar CM, Arend R, Barber E, Bradley K, Brooks R, Campos SM, Chino J, Chon HS, Crispens MA, Damast S, Fisher CM, Frederick P, Gaffney DK, Gaillard S, Giuntoli R, Glaser S, Holmes J, Howitt BE, Lea J, Mantia-Smaldone G, Mariani A, Mutch D, Nagel C, Nekhlyudov L, Podoll M, Rodabaugh K, Salani R, Schorge J, Siedel J, Sisodia R, Soliman P, Ueda S, Urban R, Wyse E, McMillian NR, Aggarwal S, Espinosa S
2023 Dec;21(12):1224-1233. doi: 10.6004/jnccn.2023.0062.
-
More
The NCCN Guidelines for Cervical Cancer provide recommendations for all aspects of management for cervical cancer, including the diagnostic workup, staging, pathology, and treatment. The guidelines also include details on histopathologic classification of cervical cancer regarding diagnostic features, molecular profiles, and clinical outcomes. The treatment landscape of advanced cervical cancer is evolving constantly. These NCCN Guidelines Insights provide a summary of recent updates regarding the systemic therapy recommendations for recurrent or metastatic disease.
PMID:38081139 | DOI:10.6004/jnccn.2023.0062
View details for PubMedID 38081139
-
More
-
The role of ctDNA in endometrial cancer: A tool for risk stratification and disease monitoring Gynecologic oncology
Blitzer GC, Zhao SG, Bradley KA, Hartenbach EM
2023 Nov;178:170-171. doi: 10.1016/j.ygyno.2023.08.008. Epub 2023 Aug 28.
-
TCR-α/β and CD19 depleted stem cell grafts from haploidentical donors for allogeneic transplantation in patients with relapsed lymphoma: a single-center experience Leukemia & lymphoma
Kenkre VP, Bradley K, Milton A, Burkholder JK, Grindle K, McMannes J, Kim K, Callander N, Juckett M, Longo W, Hematti P
2023 Nov-Dec;64(11):1875-1879. doi: 10.1080/10428194.2023.2240918. Epub 2023 Aug 10.
-
Effect of COVID-19 on Gynecologic Oncology Care: A Survey of Practicing Gynecologic Radiation Oncologists in the United States Advances in radiation oncology
Brower JV, Rhodes SS, Remick JS, Russo AL, Dunn EF, Ayala-Peacock DN, Petereit DG, Bradley KA, Taunk NK
2023 Jul-Aug;8(4):101188. doi: 10.1016/j.adro.2023.101188. Epub 2023 Feb 26.
-
More
PURPOSE: The COVID-19 pandemic has placed demands and limitations on the delivery of health care. We sought to assess the effect of COVID-19 on the delivery of gynecologic oncologic care from the perspective of practicing radiation oncologists in the United States.
METHODS AND MATERIALS: An anonymous online survey was created and distributed to preidentified radiation oncologists in the United States with clinical expertise in the management of gynecologic patients. The survey consisted of demographic questions followed by directed questions to assess specific patterns of care related to the COVID-19 pandemic.
RESULTS: A total of 47 of 96 invited radiation oncologists responded to the survey for a response rate of 49%. Fifty-six percent of respondents reported an increase in locally advanced cervical cancer with no similar increase for endometrial, vulvar, or vaginal patients. Most respondents (66%) reported a pause in surgical management, with a duration of 1 to 3 months being most common (61%). There was a reported increased use of shorter brachytherapy regimens during the pandemic. Most providers (61%) reported caring for at least 1 patient with a positive COVID-19 test. A pause or delay in treatment due to COVID-19 positivity was reported by 45% of respondents, with 55% reporting that patients chose to delay their own care because of COVID-19-related concerns. Total treatment times >8 weeks for patients with cervical cancer were observed by 33% of respondents, but occurred in >25% of patients.
CONCLUSIONS: Data from this prospectively collected anonymous survey of practice patterns among radiation oncologists reveal that the COVID-19 pandemic resulted in delays initiating care, truncated brachytherapy treatment courses, and a reported increase in locally advanced cervical cancer cases at presentation. These data can be used as a means of self-assessment to ensure appropriate decision making for gynecologic patients during the endemic phase of COVID-19.
PMID:36974086 | PMC:PMC9968481 | DOI:10.1016/j.adro.2023.101188
View details for PubMedID 36974086
-
More
-
Uterine Neoplasms, Version 1.2023, NCCN Clinical Practice Guidelines in Oncology Journal of the National Comprehensive Cancer Network : JNCCN
Abu-Rustum N, Yashar C, Arend R, Barber E, Bradley K, Brooks R, Campos SM, Chino J, Chon HS, Chu C, Crispens MA, Damast S, Fisher CM, Frederick P, Gaffney DK, Giuntoli R, Han E, Holmes J, Howitt BE, Lea J, Mariani A, Mutch D, Nagel C, Nekhlyudov L, Podoll M, Salani R, Schorge J, Siedel J, Sisodia R, Soliman P, Ueda S, Urban R, Wethington SL, Wyse E, Zanotti K, McMillian NR, Aggarwal S
2023 Feb;21(2):181-209. doi: 10.6004/jnccn.2023.0006.
-
More
Adenocarcinoma of the endometrium (also known as endometrial cancer, or more broadly as uterine cancer or carcinoma of the uterine corpus) is the most common malignancy of the female genital tract in the United States. It is estimated that 65,950 new uterine cancer cases will have occurred in 2022, with 12,550 deaths resulting from the disease. Endometrial carcinoma includes pure endometrioid cancer and carcinomas with high-risk endometrial histology (including uterine serous carcinoma, clear cell carcinoma, carcinosarcoma [also known as malignant mixed Müllerian tumor], and undifferentiated/dedifferentiated carcinoma). Stromal or mesenchymal sarcomas are uncommon subtypes accounting for approximately 3% of all uterine cancers. This selection from the NCCN Guidelines for Uterine Neoplasms focuses on the diagnosis, staging, and management of pure endometrioid carcinoma. The complete version of the NCCN Guidelines for Uterine Neoplasms is available online at NCCN.org.
PMID:36791750 | DOI:10.6004/jnccn.2023.0006
View details for PubMedID 36791750
-
More
-
Local Graft Irradiation for Acute, Medication Refractory Transplant Rejection of a Pancreas Alone Graft: A Case Report Advances in radiation oncology
Morris BA, Alfson A, Davies G, Kaufman D, Bradley KA
2022 Dec 30;8(2):101168. doi: 10.1016/j.adro.2022.101168. eCollection 2023 Mar-Apr.
-
Management of Radiographically Positive Pelvic and/or Para-aortic Lymph Nodes During Primary Chemoradiation Therapy for Cervix Cancer Practical radiation oncology
Brower JV, Bradley KA, Russo AL
2023 May-Jun;13(3):246-250. doi: 10.1016/j.prro.2022.11.010. Epub 2022 Dec 16.
-
Radiation Therapy for Endometrial Cancer: An American Society for Radiation Oncology Clinical Practice Guideline Practical radiation oncology
Harkenrider MM, Abu-Rustum N, Albuquerque K, Bradfield L, Bradley K, Dolinar E, Doll CM, Elshaikh M, Frick MA, Gehrig PA, Han K, Hathout L, Jones E, Klopp A, Mourtada F, Suneja G, Wright AA, Yashar C, Erickson BA
2023 Jan-Feb;13(1):41-65. doi: 10.1016/j.prro.2022.09.002. Epub 2022 Oct 22.
-
More
PURPOSE: With the results of several recently published clinical trials, this guideline informs on the use of adjuvant radiation therapy (RT) and systemic therapy in the treatment of endometrial cancer. Updated evidence-based recommendations provide indications for adjuvant RT and the associated techniques, the utilization and sequencing of adjuvant systemic therapies, and the effect of surgical staging techniques and molecular tumor profiling.
METHODS: The American Society for Radiation Oncology convened a multidisciplinary task force to address 6 key questions that focused on the adjuvant management of patients with endometrial cancer. The key questions emphasized the (1) indications for adjuvant RT, (2) RT techniques, target volumes, dose fractionation, and treatment planning aims, (3) indications for systemic therapy, (4) sequencing of systemic therapy with RT, (5) effect of lymph node assessment on utilization of adjuvant therapy, and (6) effect of molecular tumor profiling on utilization of adjuvant therapy. Recommendations were based on a systematic literature review and created using a predefined consensus-building methodology and system for quality of evidence grading and strength of recommendation.
RESULTS: The task force recommends RT (either vaginal brachytherapy or external beam RT) be given based on the patient's clinical-pathologic risk factors to reduce risk of vaginal and/or pelvic recurrence. When external beam RT is delivered, intensity modulated RT with daily image guided RT is recommended to reduce acute and late toxicity. Chemotherapy is recommended for patients with International Federation of Gynecology and Obstetrics (FIGO) stage I to II with high-risk histologies and those with FIGO stage III to IVA with any histology. When sequencing chemotherapy and RT, there is no prospective data to support an optimal sequence. Sentinel lymph node mapping is recommended over pelvic lymphadenectomy for surgical nodal staging. Data on sentinel lymph node pathologic ultrastaging status supports that patients with isolated tumor cells be treated as node negative and adjuvant therapy based on uterine risk factors and patients with micrometastases be treated as node positive. The available data on molecular characterization of endometrial cancer are compelling and should be increasingly considered when making recommendations for adjuvant therapy.
CONCLUSIONS: These recommendations guide evidence-based best clinical practices on the use of adjuvant therapy for endometrial cancer.
PMID:36280107 | DOI:10.1016/j.prro.2022.09.002
View details for PubMedID 36280107
-
More
-
Targeting the GTV in medically inoperable endometrial cancer using brachytherapy Brachytherapy
Merfeld EC, Kuczmarska-Haas A, Burr AR, Witt JS, Francis DM, Ntambi J, Desai VK, Huang JY, Miller JR, Lawless MJ, Wallace CR, Anderson BM, Bradley KA
2022 Nov-Dec;21(6):792-798. doi: 10.1016/j.brachy.2022.07.006. Epub 2022 Aug 24.
-
More
PURPOSE: We aimed to determine the relationship between gross tumor volume (GTV) dose and tumor control in women with medically inoperable endometrial cancer, and to demonstrate the feasibility of targeting a GTV-focused volume using imaged-guided brachytherapy.
METHODS AND MATERIALS: An endometrial cancer database was used to identify patients. Treatment plans were reviewed to determine doses to GTV, clinical target volume (CTV), and OARs. Uterine recurrence-free survival was evaluated as a function of CTV and GTV doses. Brachytherapy was replanned with a goal of GTV D98 EQD2 ≥ 80 Gy, without regard for coverage of the uninvolved uterus and while respecting OAR dose constraints.
RESULTS: Fifty-four patients were identified. In the delivered plans, GTV D90 EQD2 ≥ 80 Gy was achieved in 36 (81.8%) patients. Uterine recurrence-free survival was 100% in patients with GTV D90 EQD2 ≥ 80 Gy and 66.7% in patients with EQD2 < 80 Gy (p = 0.001). On GTV-only replans, GTV D98 EQD2 ≥ 80 Gy was achieved in 39 (88.6%) patients. Mean D2cc was lower for bladder (47.1 Gy vs. 73.0 Gy, p < 0.001), and sigmoid (47.0 Gy vs. 58.0 Gy, p = 0.007) on GTV-only replans compared to delivered plans. Bladder D2cc was ≥ 80 Gy in 11 (25.0%) delivered plans and four (9.1%) GTV-only replans (p = 0.043). Sigmoid D2cc was ≥ 65 Gy in 20 (45.4%) delivered plans and 10 (22.7%) GTV-only replans (p = 0.021).
CONCLUSIONS: OAR dose constraints should be prioritized over CTV coverage if GTV coverage is sufficient. Prospective evaluation of image-guided brachytherapy to a reduced, GTV-focused volume is warranted.
PMID:36030167 | DOI:10.1016/j.brachy.2022.07.006
View details for PubMedID 36030167
-
More
-
NCCN Guidelines® Insights: Uterine Neoplasms, Version 3.2021 Journal of the National Comprehensive Cancer Network : JNCCN
Abu-Rustum NR, Yashar CM, Bradley K, Campos SM, Chino J, Chon HS, Chu C, Cohn D, Crispens MA, Damast S, Diver E, Fisher CM, Frederick P, Gaffney DK, George S, Giuntoli R, Han E, Howitt B, Huh WK, Lea J, Mariani A, Mutch D, Nekhlyudov L, Podoll M, Remmenga SW, Reynolds RK, Salani R, Sisodia R, Soliman P, Tanner E, Ueda S, Urban R, Wethington SL, Wyse E, Zanotti K, McMillian NR, Motter AD
2021 Aug 1;19(8):888-895. doi: 10.6004/jnccn.2021.0038.
-
More
The NCCN Guidelines for Uterine Neoplasms provide recommendations for diagnostic workup, clinical staging, and treatment options for patients with endometrial cancer or uterine sarcoma. These NCCN Guidelines Insights focus on the recent addition of molecular profiling information to aid in accurate diagnosis, classification, and treatment of uterine sarcomas.
PMID:34416706 | DOI:10.6004/jnccn.2021.0038
View details for PubMedID 34416706
-
More
-
Four Ways to Decrease Late Toxicity From Pelvic Radiation Therapy in Children and Young Adults Practical radiation oncology
Blitzer GC, Bradley KA
2021 Nov-Dec;11(6):434-440. doi: 10.1016/j.prro.2021.07.001. Epub 2021 Jul 16.
-
More
The use of curative-intent multimodality therapy with chemotherapy, surgery, and radiation results in late toxicities in almost two-thirds of patients with pediatric cancer. When pelvic radiation is used for pediatric malignancies such as rhabdomyosarcoma, lymphoma, neuroblastoma, Ewing sarcoma, and Wilms tumor, the associated late toxicities can affect many normal tissues and may include growth asymmetries, cystitis, infertility, and sexual dysfunction. We describe 4 recommendations of how to prevent or minimize late toxicities from pelvic radiation and review the literature of these pediatric late toxicities.
PMID:34274520 | DOI:10.1016/j.prro.2021.07.001
View details for PubMedID 34274520
-
More
-
Sustained Increase of Sedative-Hypnotic Prescribing During the COVID-19 Pandemic in a Large Urban Health System: an Observational Study Journal of general internal medicine
Keller MS, Kiefer E, Campbell S, Bradley K, Mashburn R, Bawa M, Goldzweig C
2021 Nov;36(11):3618-3620. doi: 10.1007/s11606-021-06868-5. Epub 2021 May 13.
-
Rare tumors: Retinoblastoma, nasopharyngeal cancer, and adrenocorticoid tumors Pediatric blood & cancer
Patel S, Vogel J, Bradley K, Chuba PJ, Buchsbaum J, Krasin MJ
2021 May;68 Suppl 2:e28253. doi: 10.1002/pbc.28253.
-
More
The role of surgery, chemotherapy, and radiation therapy for retinoblastoma has evolved considerably over the years with the efficacy of intraarterial chemotherapy and the high incidence of secondary malignant neoplasms following radiation therapy. The use of spot scanning intensity-modulated proton therapy may reduce the risk of secondary malignancies. For pediatric nasopharyngeal carcinoma, the current standard of care is induction chemotherapy followed by chemoradiation therapy. For adrenocortical carcinoma, the mainstay of treatment is surgery and chemotherapy. The role of radiation therapy remains to be defined.
PMID:33818883 | DOI:10.1002/pbc.28253
View details for PubMedID 33818883
-
More
-
Comparison of catheter reconstruction techniques for the lunar ovoid channels of the Venezia<sup>TM</sup> applicator Journal of contemporary brachytherapy
Hansen J, Dunkerley D, Bradley K, Miller J, Huang J
2020 Aug;12(4):383-392. doi: 10.5114/jcb.2020.98119. Epub 2020 Aug 21.
-
More
PURPOSE: The aim of this study was to compare catheter reconstruction methods for lunar ovoid channels of the VeneziaTM advanced gynecological applicator (Elekta, Sweden).
MATERIAL AND METHODS: Three available lunar ovoid sizes (22, 26, and 30 mm effective diameter) were evaluated. Computed tomography (CT) scans were performed with a dummy wire inserted and with the Flexitron® source position simulator (SPS) at step sizes of 5 mm from the most distal dwell position. Treatment plans were generated in Oncentra® (version 4.5.3) with different catheter reconstruction techniques: centerline reconstruction, tracing a CT dummy wire, using a source path model provided by Elekta, and using the SPS at each planning dwell position. Source position agreement was assessed in registered CT images, and dose differences were calculated with the SPS-based treatment plan as a reference. Finally, dose-volume histogram (DVH) parameters were evaluated for clinical plans with the VeneziaTM applicator.
RESULTS: For the most distal dwell position, the manufacturer's model had the closest agreement with the SPS at 0.6 ±0.3 mm across applicator sizes. Relative to the SPS, maximal dose differences outside of the applicator were between 16-39% for a 0.1 cm3 volume and 3.6-9.1% for a 2.0 cm3 volume. For two clinical plans, volume-based DVH parameters agreed ≤ 3.9%, while deviations ≤ 5.3% were seen for point metrics.
CONCLUSIONS: Relative to the SPS-based plan, large local dose discrepancies were reduced, but not eliminated, using the manufacturer's source path model. The choice of reconstruction technique was found to have relatively limited impact on DVH parameters for regions outside of the vaginal mucosa.
PMID:33293978 | PMC:PMC7690228 | DOI:10.5114/jcb.2020.98119
View details for PubMedID 33293978
-
More
-
NCCN Guidelines Insights: Cervical Cancer, Version 1.2020 Journal of the National Comprehensive Cancer Network : JNCCN
Abu-Rustum NR, Yashar CM, Bean S, Bradley K, Campos SM, Chon HS, Chu C, Cohn D, Crispens MA, Damast S, Fisher CM, Frederick P, Gaffney DK, Giuntoli R, Han E, Huh WK, Iii RL, Mariani A, Mutch D, Nagel C, Nekhlyudov L, Fader AN, Remmenga SW, Reynolds RK, Sisodia R, Tillmanns T, Ueda S, Urban R, Wyse E, McMillian NR, Motter AD
2020 Jun;18(6):660-666. doi: 10.6004/jnccn.2020.0027.
-
More
The NCCN Guidelines for Cervical Cancer provide recommendations for diagnostic workup, staging, and treatment of patients with the disease. These NCCN Guidelines Insights focus on recent updates to the guidelines, including changes to first- and second-line systemic therapy recommendations for patients with recurrent or metastatic disease, and emerging evidence on a new histopathologic classification system for HPV-related endocervical adenocarcinoma.
PMID:32502976 | DOI:10.6004/jnccn.2020.0027
View details for PubMedID 32502976
-
More
-
Gestational Trophoblastic Neoplasia, Version 2.2019, NCCN Clinical Practice Guidelines in Oncology Journal of the National Comprehensive Cancer Network : JNCCN
Abu-Rustum NR, Yashar CM, Bean S, Bradley K, Campos SM, Chon HS, Chu C, Cohn D, Crispens MA, Damast S, Dorigo O, Eifel PJ, Fisher CM, Frederick P, Gaffney DK, Han E, Huh WK, Lurain JR, Mariani A, Mutch D, Nagel C, Nekhlyudov L, Fader AN, Remmenga SW, Reynolds RK, Sisodia R, Tillmanns T, Ueda S, Wyse E, McMillian NR, Scavone J
2019 Nov 1;17(11):1374-1391. doi: 10.6004/jnccn.2019.0053.
-
More
Gestational trophoblastic neoplasia (GTN), a subset of gestational trophoblastic disease (GTD), occurs when tumors develop in the cells that would normally form the placenta during pregnancy. The NCCN Guidelines for Gestational Trophoblastic Neoplasia provides treatment recommendations for various types of GTD including hydatidiform mole, persistent post-molar GTN, low-risk GTN, high-risk GTN, and intermediate trophoblastic tumor.
PMID:31693991 | DOI:10.6004/jnccn.2019.0053
View details for PubMedID 31693991
-
More
-
Combining brachytherapy and immunotherapy to achieve in situ tumor vaccination: A review of cooperative mechanisms and clinical opportunities Brachytherapy
Patel RB, Baniel CC, Sriramaneni RN, Bradley K, Markovina S, Morris ZS
2019 Mar-Apr;18(2):240. doi: 10.1016/j.brachy.2019.01.004.
-
Cervical Cancer, Version 3.2019, NCCN Clinical Practice Guidelines in Oncology Journal of the National Comprehensive Cancer Network : JNCCN
Koh W, Abu-Rustum NR, Bean S, Bradley K, Campos SM, Cho KR, Chon HS, Chu C, Clark R, Cohn D, Crispens MA, Damast S, Dorigo O, Eifel PJ, Fisher CM, Frederick P, Gaffney DK, Han E, Huh WK, Lurain JR, Mariani A, Mutch D, Nagel C, Nekhlyudov L, Fader AN, Remmenga SW, Reynolds RK, Tillmanns T, Ueda S, Wyse E, Yashar CM, McMillian NR, Scavone JL
2019 Jan;17(1):64-84. doi: 10.6004/jnccn.2019.0001.
-
More
Cervical cancer is a malignant epithelial tumor that forms in the uterine cervix. Most cases of cervical cancer are preventable through human papilloma virus (HPV) vaccination, routine screening, and treatment of precancerous lesions. However, due to inadequate screening protocols in many regions of the world, cervical cancer remains the fourth-most common cancer in women globally. The complete NCCN Guidelines for Cervical Cancer provide recommendations for the diagnosis, evaluation, and treatment of cervical cancer. This manuscript discusses guiding principles for the workup, staging, and treatment of early stage and locally advanced cervical cancer, as well as evidence for these recommendations. For recommendations regarding treatment of recurrent or metastatic disease, please see the full guidelines on NCCN.org.
PMID:30659131 | DOI:10.6004/jnccn.2019.0001
View details for PubMedID 30659131
-
More
-
Validity and reliability pilot study of a tool for assessing ambulatory care pharmacist practice American journal of health-system pharmacy : AJHP : official journal of the American Society of Health-System Pharmacists
Bradley KD, Schumacher C, Borchert JS, Kliethermes MA, Anderson DK
2018 Dec 1;75(23):1890-1901. doi: 10.2146/ajhp170678. Epub 2018 Oct 17.
-
More
PURPOSE: The reliability and validity of a survey tool that aims to assess and stratify patient care services provided by ambulatory care pharmacists were evaluated.
METHODS: The Tool for Assessing Ambulatory Care Pharmacist Practice (TAAPP) was developed by updating the Pharmaceutical Care Clinical Pharmacist Questionnaire. The TAAPP is organized into 2 sections that include 5 domains derived from the Pharmacists' Patient Care Process (PPCP). The first section of the TAAPP gathers the demographic information of the respondents as well as practice site characteristics. The second section aims to assess the activities that ambulatory care pharmacists participate in when providing direct patient care, stratified by PPCP domains. After the TAAPP was created, face validity was established by the study investigators and content validity was confirmed by 5 experts in ambulatory care pharmacy. Lastly, a reliability study was conducted and included pharmacists providing ambulatory care services in outpatient clinics who had been working at their clinical practice site for at least 2 years. The survey was disseminated electronically through a national pharmacy organization listserver.
RESULTS: The results of this pilot study support both face and content validity of the TAAPP survey as well as internal consistency reliability of the TAAPP scores when used to evaluate pharmaceutical practices of ambulatory care pharmacists practicing in outpatient clinics throughout the United States.
CONCLUSION: Internal consistency reliability testing demonstrated that the TAAPP scores were reliable with a Cronbach's α of >0.7 for each domain and the TAAPP overall.
PMID:30333111 | DOI:10.2146/ajhp170678
View details for PubMedID 30333111
-
More
-
In Reply to Lin and Golden International journal of radiation oncology, biology, physics
Jang S, Rosenberg SA, Bradley KA, Kimple RJ
2018 Nov 1;102(3):672. doi: 10.1016/j.ijrobp.2018.06.043.
-
Combining brachytherapy and immunotherapy to achieve in situ tumor vaccination: A review of cooperative mechanisms and clinical opportunities Brachytherapy
Patel RB, Baniel CC, Sriramaneni RN, Bradley K, Markovina S, Morris ZS
2018 Nov-Dec;17(6):995-1003. doi: 10.1016/j.brachy.2018.07.004. Epub 2018 Aug 2.
-
More
As immunotherapies continue to emerge as a standard component of treatment for a variety of cancers, the imperative for testing these in combination with other standard cancer therapies grows. Radiation therapy may be a particularly well-suited partner for many immunotherapies. By modulating immune tolerance and functional immunogenicity at a targeted tumor site, radiation therapy may serve as a method of in situ tumor vaccination. In situ tumor vaccination is a therapeutic strategy that seeks to convert a patient's own tumor into a nidus for enhanced presentation of tumor-specific antigens in a way that will stimulate and diversify an antitumor T cell response. The mechanisms whereby radiation may impact immunotherapy are diverse and include its capacity to simultaneously elicit local inflammation, temporary local depletion of suppressive lymphocyte lineages, enhanced tumor cell susceptibility to immune response, and immunogenic tumor cell death. Emerging data suggest that each of these mechanisms may display a distinct dose-response profile, making it challenging to maximize each of these effects using external beam radiation. Conversely, the highly heterogenous and conformal dose distribution achieved with brachytherapy may be optimal for enhancing the immunogenic capacity of radiation at a tumor site while minimizing off-target antagonistic effects on peripheral immune cells. Here, we review the immunogenic effects of radiation, summarize the clinical rationale and data supporting the use of radiation together with immunotherapies, and discuss the rationale and urgent need for further preclinical and clinical investigation specifically of brachytherapy in combination with immunotherapies. Harnessing these immunomodulatory effects of brachytherapy may offer solutions to overcome obstacles to the efficacy of immunotherapies in immunologically "cold" tumors while potentiating greater response in the context of immunologically "hot" tumors.
PMID:30078541 | PMC:PMC8292980 | DOI:10.1016/j.brachy.2018.07.004
View details for PubMedID 30078541
-
More
-
Beyond 'charting outcomes' in the radiation oncology match: analysis of self-reported applicant data Medical education online
Jang S, Rosenberg SA, Hullett C, Bradley KA, Kimple RJ
2018 Dec;23(1):1489691. doi: 10.1080/10872981.2018.1489691.
-
More
The Charting Outcomes resource is useful in gauging an applicant's competiveness for a given specialty. However, many variables are not reported in Charting Outcomes that may influence an applicant's ability to match. A significant proportion of applicants record their experiences in an anonymous, self-reported applicant spreadsheet. We analyzed factors associated with a successful match using this dataset to test the hypothesis that research productivity and high academic performance correlates with success rates. A retrospective analysis of "RadOnc Interview Spreadsheet" for the 2015, 2016, and 2017 radiation oncology match was performed. Data were accessed via studentdoctor.net. Board scores, research characteristics, Sub-I participation, and interview invitation rates were available. Mann-Whitney U, Kruskal-Wallis, and chi-square tests were used for statistical analysis. When possible, results were compared to those reported in the National Residency Match Program's "Charting Outcomes" report. A total of 158 applicants were examined for the applicant characteristics. Applicants applied to a median of 61 programs and received a median of 14 interviews. The mean step 1 score was 248 (range: 198 to 272) and most were in the highest grade point average quartile (68.3%). 21.7% participated in additional research year(s), and 19% obtained a PhD. The majority of applicants took three radiation oncology electives (48.7%). On multivariate analysis, alpha-omega-alpha (AOA) honors society status (p=0.033), participating in a research year (p=0.001) and number of journal publications (p=0.047) significantly correlated with higher interview invitation rates. In summary, this study identifies important considerations for radiation oncology applicants that have not been previously reported, such as induction into AOA and number of journal publications.
PMID:29943670 | PMC:PMC6022246 | DOI:10.1080/10872981.2018.1489691
View details for PubMedID 29943670
-
More
-
Objective Evaluation of a Didactic Curriculum for the Radiation Oncology Medical Student Clerkship International journal of radiation oncology, biology, physics
Golden DW, Kauffmann GE, McKillip RP, Farnan JM, Park YS, Schwartz A, Group CS
2018 Aug 1;101(5):1039-1045. doi: 10.1016/j.ijrobp.2018.04.052. Epub 2018 Apr 26.
-
More
PURPOSE: A structured didactic radiation oncology clerkship curriculum for medical students is in use at multiple academic medical centers. Objective evidence supporting this educational approach over the traditional clerkship model is lacking. This study evaluated the curriculum efficacy using an objective knowledge assessment.
METHODS AND MATERIALS: Medical students received the Radiation Oncology Education Collaborative Study Group (ROECSG) curriculum consisting of 3 lectures (Overview of Radiation Oncology, Radiation Biology/Physics, and Practical Aspects of Simulation/Radiation Emergencies) and a radiation oncology treatment-planning workshop. A standardized 20-item multiple choice question (MCQ) knowledge assessment was completed pre- and post-curriculum and approximately 6 months after receiving the curriculum.
RESULTS: One hundred forty-six students at 22 academic medical centers completed the ROECSG curriculum from July to November 2016. One hundred nine students completed pre- and post-clerkship MCQ knowledge assessments (response rate 74.7%). Twenty-four students reported a prior rotation at a ROECSG institution and were excluded from analysis. Mean assessment scores increased from pre- to post-curriculum (63.9% vs 80.2%, P < .01). Mean MCQ knowledge subdomain assessment scores all improved post-curriculum (t test, P values < .01). Post-scores for students rotating de novo at ROECSG institutions (n = 30) were higher compared with pre-scores for students with ≥1 prior rotations at non-ROECSG institutions (n = 55) (77.3% vs 68.8%, P = .01), with an effect size of 0.8. Students who completed rotations at ROECSG institutions continued to demonstrate a trend toward improved performance on the objective knowledge assessment at approximately 6 months after curriculum exposure (70.5% vs 65.6%, P = .11).
CONCLUSIONS: Objective evaluation of a structured didactic curriculum for the radiation oncology clerkship at early and late time points demonstrated significant improvement in radiation oncology knowledge. Students who completed clerkships at ROECSG institutions performed objectively better than students who completed clerkships at non-ROECSG institutions. These results support including a structured didactic curriculum as a standard component of the radiation oncology clerkship.
PMID:29908787 | PMC:PMC6538302 | DOI:10.1016/j.ijrobp.2018.04.052
View details for PubMedID 29908787
-
More
-
A New Era of Image Guidance with Magnetic Resonance-guided Radiation Therapy for Abdominal and Thoracic Malignancies Cureus
Mittauer K, Paliwal B, Hill P, Bayouth JE, Geurts MW, Baschnagel AM, Bradley KA, Harari PM, Rosenberg S, Brower JV, Wojcieszynski AP, Hullett C, Bayliss RA, Labby ZE, Bassetti MF
2018 Apr 4;10(4):e2422. doi: 10.7759/cureus.2422.
-
More
Magnetic resonance-guided radiation therapy (MRgRT) offers advantages for image guidance for radiotherapy treatments as compared to conventional computed tomography (CT)-based modalities. The superior soft tissue contrast of magnetic resonance (MR) enables an improved visualization of the gross tumor and adjacent normal tissues in the treatment of abdominal and thoracic malignancies. Online adaptive capabilities, coupled with advanced motion management of real-time tracking of the tumor, directly allow for high-precision inter-/intrafraction localization. The primary aim of this case series is to describe MR-based interventions for localizing targets not well-visualized with conventional image-guided technologies. The abdominal and thoracic sites of the lung, kidney, liver, and gastric targets are described to illustrate the technological advancement of MR-guidance in radiotherapy.
PMID:29872602 | PMC:PMC5985918 | DOI:10.7759/cureus.2422
View details for PubMedID 29872602
-
More
-
Novel use of ViewRay MRI guidance for high-dose-rate brachytherapy in the treatment of cervical cancer Brachytherapy
Ko HC, Huang JY, Miller JR, Das RK, Wallace CR, Costa AD, Francis DM, Straub MR, Anderson BM, Bradley KA
2018 Jul-Aug;17(4):680-688. doi: 10.1016/j.brachy.2018.04.005. Epub 2018 Jun 7.
-
More
PURPOSE: To characterize image quality and feasibility of using ViewRay MRI (VR)-guided brachytherapy planning for cervical cancer.
METHODS AND MATERIALS: Cervical cancer patients receiving intracavitary brachytherapy with tandem and ovoids, planned using 0.35T VR MRI at our institution, were included in this series. The high-risk clinical target volume (HR-CTV), visible gross tumor volume, bladder, sigmoid, bowel, and rectum contours for each fraction of brachytherapy were evaluated for dosimetric parameters. Typically, five brachytherapy treatments were planned using the T2 sequence on diagnostic MRI for the first and third fractions, and a noncontrast true fast imaging with steady-state precession sequence on VR or CT scan for the remaining fractions. Most patients received 5.5 Gy × 5 fractions using high-dose-rate Ir-192 following 45 Gy of whole-pelvis radiotherapy. The plan was initiated at 5.5 Gy to point A and subsequently optimized and prescribed to the HR-CTV. The goal equivalent dose in 2 Gy fractions for the combined external beam and brachytherapy dose was 85 Gy. Soft-tissue visualization using contrast-to-noise ratios to distinguish normal tissues from tumor at their interface was compared between diagnostic MRI, CT, and VR.
RESULTS: One hundred and forty-two fractions of intracavitary brachytherapy were performed from April 2015 to January 2017 on 29 cervical cancer patients, ranging from stages IB1 to IVA. The median HR-CTV was 27.78 cc, with median D90 HR-CTV of 6.1 Gy. The median time from instrument placement to start of treatment using VR was 65 min (scan time 2 min), compared to 105 min using diagnostic MRI (scan time 11 min) (t-test, p < 0.01). The contrast-to-noise ratio of tumor to cervix in both diagnostic MRI and VR had significantly higher values compared to CT (ANOVA and t-tests, p < 0.01).
CONCLUSIONS: We report the first clinical use of VR-guided brachytherapy. Time to treatment using this approach was shorter compared to diagnostic MRI. VR also provided significant advantage in visualizing the tumor and cervix compared to CT. This presents a feasible and reliable manner to image and plan gynecologic brachytherapy.
PMID:29773331 | DOI:10.1016/j.brachy.2018.04.005
View details for PubMedID 29773331
-
More
-
In Reply to Hamstra International journal of radiation oncology, biology, physics
Rosenberg SA, Bradley KA, Kimple RJ
2018 Apr 1;100(5):1293-1294. doi: 10.1016/j.ijrobp.2018.01.038.
-
The role of radiation therapy in the treatment of Stage II endometrial cancer: A large database study Brachytherapy
Wojcieszynski AP, Hullett CR, Medlin EE, Taunk NK, Shabason JE, Brower JV, Chen S, Bekelman JE, Barroilhet LM, Bradley KA
2018 Jul-Aug;17(4):645-652. doi: 10.1016/j.brachy.2018.02.001. Epub 2018 Apr 22.
-
More
PURPOSE: The optimum adjuvant treatment for Stage II endometrial cancer patients is unknown. External beam radiation therapy (EBRT) is often considered the standard of care; however, retrospective series suggest that brachytherapy (BT) alone may be sufficient for selected patients. As randomized data are lacking, we used a large database to explore this question.
METHODS AND MATERIALS: The National Cancer Data Base was queried for patients with pathologic International Federation of Gynecology and Obstetrics Stage II disease. Demographic, clinic-pathologic, and treatment details were compared between patients. Multivariable analysis was used to determine factors associated with receiving radiation therapy (RT). To account for imbalances between groups, a matched-pair analysis was completed.
RESULTS: Eight thousand one hundred forty patients were included. RT was associated with overall survival (OS), with EBRT (hazard ratio [HR] 0.64), BT (HR 0.47), and combination (HR 0.54) showing increased OS on univariate analysis. Facility, urban location, diagnosis year, hysterectomy type, and chemotherapy did not reach significance. On multivariate analysis, RT was associated with OS, with EBRT (HR 0.69), BT (HR 0.60), and combination (HR 0.54) showing benefit. Using propensity-score matching, RT continued to show improved OS regardless of type: BT (82% vs. 73% 5-year OS) and EBRT (77% vs. 71%). BT as compared to EBRT had equivalent survival (81% vs. 79%, not statistically significant).
CONCLUSION: This study of over 8,000 patients demonstrates that adjuvant RT confers a survival benefit in Stage II endometrial cancer and supports the continued use of RT in these patients. BT alone may be reasonable in carefully selected patients.
PMID:29691149 | DOI:10.1016/j.brachy.2018.02.001
View details for PubMedID 29691149
-
More
-
Bone marrow suppression as a complication of total skin helical tomotherapy in the treatment of mycosis fungoides Radiation oncology (London, England)
Schaff EM, Rosenberg SA, Olson SJ, Howard SP, Bradley KA
2018 Apr 13;13(1):67. doi: 10.1186/s13014-018-1013-2.
-
More
BACKGROUND: Total skin electron beam therapy (TSEBT) is an effective treatment in mycosis fungoides. Total skin helical tomotherapy (TSHT) may be an alternative to TSEBT and may offer several dosimetric and treatment advantages. There are currently very few published treatment results using TSHT in place of TSEBT for treatment of mycosis fungoides.
CASE PRESENTATION: Two patients with mycosis fungoides were treated at our institution using TSHT. The first patient was a 69-year-old Caucasian female with stage IVA2 (T2 N3 M0 B2) disease who was treated to a dose of 12 Gy in 8 fractions, with a bone marrow mean dose of 1.66 Gy and V10 = 0.41%. Two weeks after ending treatment the patient developed myelosuppression including grade 4 thrombocytopenia and required blood and platelet transfusions. The second patient was a 29-year-old Caucasian female with stage I (T2 N0 M0 B0) disease. This patient previously had been treated for mycosis fungoides using helical tomotherapy (HT) at a dose of 20 Gy to a localized region and experienced mild thrombocytopenia at that time. The patient then underwent retreatment 17 months later with TSHT to a dose of 12 Gy in 6 fractions with a mean bone marrow dose of 2.3 Gy and V10 = 4.28%. This patient once again experienced myelosuppression that included grade 4 thrombocytopenia. She also required blood and platelet transfusions.
CONCLUSIONS: Both patients treated with TSHT experienced severe bone marrow suppression including grade 4 thrombocytopenia. This was more severe than expected considering the relatively low overall prescription dose and despite a planning constraint placed on the bone marrow of a mean dose of < 2 Gy. These outcomes suggest that patients treated using TSHT should be closely monitored for myelosuppression and caution used even when treating to a dose of 12 Gy.
PMID:29653544 | PMC:PMC5899362 | DOI:10.1186/s13014-018-1013-2
View details for PubMedID 29653544
-
More
-
Uterine Neoplasms, Version 1.2018, NCCN Clinical Practice Guidelines in Oncology Journal of the National Comprehensive Cancer Network : JNCCN
Koh W, Abu-Rustum NR, Bean S, Bradley K, Campos SM, Cho KR, Chon HS, Chu C, Cohn D, Crispens MA, Damast S, Dorigo O, Eifel PJ, Fisher CM, Frederick P, Gaffney DK, George S, Han E, Higgins S, Huh WK, Lurain JR, Mariani A, Mutch D, Nagel C, Nekhlyudov L, Fader AN, Remmenga SW, Reynolds RK, Tillmanns T, Ueda S, Wyse E, Yashar CM, McMillian NR, Scavone JL
2018 Feb;16(2):170-199. doi: 10.6004/jnccn.2018.0006.
-
More
Endometrial carcinoma is a malignant epithelial tumor that forms in the inner lining, or endometrium, of the uterus. Endometrial carcinoma is the most common gynecologic malignancy. Approximately two-thirds of endometrial carcinoma cases are diagnosed with disease confined to the uterus. The complete NCCN Guidelines for Uterine Neoplasms provide recommendations for the diagnosis, evaluation, and treatment of endometrial cancer and uterine sarcoma. This manuscript discusses guiding principles for the diagnosis, staging, and treatment of early-stage endometrial carcinoma as well as evidence for these recommendations.
PMID:29439178 | DOI:10.6004/jnccn.2018.0006
View details for PubMedID 29439178
-
More
-
Value of Elective Radiation Oncology Rotations: How Many Is Too Many? International journal of radiation oncology, biology, physics
Jang S, Rosenberg SA, Hullet C, Bradley KA, Kimple RJ
2018 Mar 1;100(3):558-559. doi: 10.1016/j.ijrobp.2017.10.052. Epub 2017 Nov 6.
-
More
PMID:29413271 | PMC:PMC5806148 | DOI:10.1016/j.ijrobp.2017.10.052
View details for PubMedID 29413271
-
More
-
Neck Rhabdoid Tumors: Clinical Features and Consideration of Autologous Stem Cell Transplant Journal of pediatric hematology/oncology
Wolfe AD, Capitini CM, Salamat SM, DeSantes K, Bradley KA, Kennedy T, Dehner LP, Patel NJ
2018 Jan;40(1):e50-e54. doi: 10.1097/MPH.0000000000000829.
-
More
Extrarenal malignant rhabdoid tumors (MRT) have a poor prognosis despite aggressive therapy. Adding high-dose chemotherapy with autologous stem cell rescue (HDC-ASCR) as consolidative therapy for MRT is controversial. We describe 2 patients, age 13 years and 19 months, with unresectable neck MRT. After chemotherapy and radiotherapy, both underwent HDC-ASCR and remain in remission over 4 years later. We reviewed all published cases of neck MRT, and found poorer outcomes and more variable age of presentation and time to progression than MRT at other sites. Neck MRT may represent a higher-risk subset of MRT, and addition of HDC-ASCR merits consideration.
PMID:28375943 | PMC:PMC5624815 | DOI:10.1097/MPH.0000000000000829
View details for PubMedID 28375943
-
More
-
Online patient information from radiation oncology departments is too complex for the general population Practical radiation oncology
Rosenberg SA, Francis DM, Hullet CR, Morris ZS, Brower JV, Anderson BM, Bradley KA, Bassetti MF, Kimple RJ
2017 Jan-Feb;7(1):57-62. doi: 10.1016/j.prro.2016.07.008. Epub 2016 Aug 1.
-
More
PURPOSE: Nearly two-thirds of cancer patients seek information about their diagnosis online. We assessed the readability of online patient education materials found on academic radiation oncology department Web sites to determine whether they adhered to guidelines suggesting that information be presented at a sixth-grade reading level.
METHODS AND MATERIALS: The Association of American Medical Colleges Web site was used to identify all academic radiation oncology departments in the United States. One-third of these department Web sites were selected for analysis using a random number generator. Both general information on radiation therapy and specific information regarding various radiation modalities were collected. To test the hypothesis that the readability of these online educational materials was written at the recommended grade level, a panel of 10 common readability tests was used. A composite grade level of readability was constructed using the 8 readability measures that provide a single grade-level output.
RESULTS: A mean of 5605 words (range, 2058-12,837) from 30 department Web sites was collected. Using the composite grade level score, the overall mean readability level was determined to be 13.36 (12.83-13.89), corresponding to a collegiate reading level. This was significantly higher than the target sixth-grade reading level (middle school, t (29) = 27.41, P < .001).
CONCLUSIONS: Online patient educational materials from academic radiation oncology Web sites are significantly more complex than recommended by the National Institutes of Health and the Department of Health and Human Services. To improve patients' comprehension of radiation therapy and its role in their treatment, our analysis suggests that the language used in online patient information should be simplified to communicate the information at a more appropriate level.
PMID:27663932 | PMC:PMC5219938 | DOI:10.1016/j.prro.2016.07.008
View details for PubMedID 27663932
-
More
-
Readability of Online Patient Educational Resources Found on NCI-Designated Cancer Center Web Sites Journal of the National Comprehensive Cancer Network : JNCCN
Rosenberg SA, Francis D, Hullett CR, Morris ZS, Fisher MM, Brower JV, Bradley KA, Anderson BM, Bassetti MF, Kimple RJ
2016 Jun;14(6):735-40. doi: 10.6004/jnccn.2016.0075.
-
More
BACKGROUND: The NIH and Department of Health & Human Services recommend online patient information (OPI) be written at a sixth grade level. We used a panel of readability analyses to assess OPI from NCI-Designated Cancer Center (NCIDCC) Web sites.
METHODS: Cancer.gov was used to identify 68 NCIDCC Web sites from which we collected both general OPI and OPI specific to breast, prostate, lung, and colon cancers. This text was analyzed by 10 commonly used readability tests: the New Dale-Chall Readability Formula, Flesch Reading Ease scale, Flesch-Kinaid Grade Level, FORCAST scale, Fry Readability Graph, Simple Measure of Gobbledygook test, Gunning Frequency of Gobbledygook index, New Fog Count, Raygor Readability Estimate Graph, and Coleman-Liau Index. We tested the hypothesis that the readability of NCIDCC OPI was written at the sixth grade level. Secondary analyses were performed to compare readability of OPI between comprehensive and noncomprehensive centers, by region, and to OPI produced by the American Cancer Society (ACS).
RESULTS: A mean of 30,507 words from 40 comprehensive and 18 noncomprehensive NCIDCCs was analyzed (7 nonclinical and 3 without appropriate OPI were excluded). Using a composite grade level score, the mean readability score of 12.46 (ie, college level: 95% CI, 12.13-12.79) was significantly greater than the target grade level of 6 (middle-school: P<.001). No difference between comprehensive and noncomprehensive centers was identified. Regional differences were identified in 4 of the 10 readability metrics (P<.05). ACS OPI provides easier language, at the seventh to ninth grade level, across all tests (P<.01).
CONCLUSIONS: OPI from NCIDCC Web sites is more complex than recommended for the average patient.
PMID:27283166 | PMC:PMC7236813 | DOI:10.6004/jnccn.2016.0075
View details for PubMedID 27283166
-
More
-
Pitfalls in Imaging of Cervical Cancer Seminars in roentgenology
Robbins J, Kusmirek J, Barroilhet L, Anderson B, Bradley K, Sadowski E
2016 Jan;51(1):17-31. doi: 10.1053/j.ro.2015.11.001. Epub 2015 Nov 26.
-
In regard to Wu and Vapiwala et al International journal of radiation oncology, biology, physics
Meyer JE, Dilling TJ, Amdur RJ, Strasser JF, Tendulkar R, Lee WR, Jani AB, Elshaikh M, Poppe MM, Takita C, Currey A, Cheng SK, Jagsi R, Kuo JV, Chen AM, Dragun AE, Bradley K, Beriwal S, Smith RP, Chen RC, Rosenzweig K, Kim S, Mehta K
2016 Mar 15;94(4):858-9. doi: 10.1016/j.ijrobp.2015.12.001.
-
Multi-Institutional Implementation and Evaluation of a Curriculum for the Medical Student Clerkship in Radiation Oncology Journal of the American College of Radiology : JACR
Committee GW, Golden DW, Braunstein S, Jimenez RB, Mohindra P, Spektor A, Ye JC, Members SG
2016 Feb;13(2):203-9. doi: 10.1016/j.jacr.2015.06.036. Epub 2015 Sep 26.
-
More
PURPOSE: Radiation oncology curriculum development is challenging because of limited numbers of trainees at any single institution. The goal of this project is to implement and evaluate a standardized medical student clerkship curriculum following the multi-institutional cooperative group research model.
METHODS: During the 2013 academic year, a standardized curriculum was implemented at 11 academic medical centers consisting of three 1-hour lectures and a hands-on radiation treatment planning workshop. After the curriculum, students completed anonymous evaluations using Likert-type scales (1 = "not at all" to 5 = "extremely") and free responses. Evaluations asked students to rate their comfort, before and after the curriculum, with radiation oncology as a specialty, knowledge of radiotherapy planning methods, and ability to function as a radiation oncology resident. Nonparametric statistical tests were used in the analysis.
RESULTS: Eighty-eight students at 11 academic medical centers completed the curriculum de novo, with a 72.7% (64 of 88) survey response rate. Fifty-seven students (89.1%) reported intent to pursue radiation oncology as their specialty. Median (interquartile range) student ratings of the importance of curricular content were as follows: overview, 4 (4-5); radiation biology/physics, 5 (4-5); practical aspects/emergencies, 5 (4-5); and planning workshop, 4 (4-5). Students reported that the curriculum helped them better understand radiation oncology as a specialty (5 [4-5]), increased specialty decision comfort (4 [3-5]), and would help the transition to radiation oncology residency (4 [4-5]). Students rated their specialty decision comfort significantly higher after completing the curriculum (4 [4-5] versus 5 [5-5]; P < .001).
CONCLUSIONS: A national standardized curriculum was successfully implemented at 11 academic medical centers, providing proof of principle that curriculum development can follow the multi-institutional cooperative group research model.
PMID:26410347 | PMC:PMC4744090 | DOI:10.1016/j.jacr.2015.06.036
View details for PubMedID 26410347
-
More
-
Medical Student Perspectives on a Multi-institutional Clerkship Curriculum: A Report From the Radiation Oncology Education Collaborative Study Group International journal of radiation oncology, biology, physics
Ye JC, Mohindra P, Spektor A, Krishnan MS, Chmura SJ, Howard AR, Viswanathan AN, MacDonald SM, Thaker NG, Das P, Mancini BR, Higgins SA, Braunstein S, Haas-Kogan D, Bradley KA, Hung AY, Thomas CR, Kharofa J, Wheatley M, Currey A, Parashar B, Du K, Jimenez RB, Golden DW
2015 Jun 1;92(2):217-9. doi: 10.1016/j.ijrobp.2015.01.043.
-
More
PMID:25968822 | PMC:PMC4768460 | DOI:10.1016/j.ijrobp.2015.01.043
View details for PubMedID 25968822
-
More
-
Impact of adjuvant pelvic radiotherapy in stage I uterine sarcoma Anticancer research
Magnuson WJ, Petereit DG, Anderson BM, Geye HM, Bradley KA
2015 Jan;35(1):365-70.
-
More
BACKGROUND/AIM: The optimal adjuvant therapy for stage I uterine sarcoma remains unresolved and may consist of radiotherapy (RT), chemotherapy, hormonal therapy or observation. We analyzed the impact of adjuvant pelvic RT on overall survival (OS), cause-specific survival (CSS), disease-free survival (DFS), pelvic control (PC) and patterns of failure.
PATIENTS AND METHODS: A retrospective analysis of 157 patients with International Federation of Gynecology and Obstetrics FIGO stage I uterine sarcoma was performed. RT was given postoperatively to a dose of 45-51 Gy in 28-30 fractions.
RESULTS: The 5-year OS, CSS, DFS and PC was 58%, 62%, 47% and 72%, respectively. Adjuvant RT significantly improved PC (85% for RT group vs. 64% for non-RT group; p=0.02) but did not impact OS, CSS or DFS.
CONCLUSION: The addition of adjuvant pelvic RT significantly improved PC for patients with stage I uterine sarcoma. As systemic therapies continue to improve, optimal locoregional control may result in improved patient outcomes.
PMID:25550573
View details for PubMedID 25550573
-
More
-
Cervical brachytherapy technique for locally advanced carcinoma of the cervix in a patient with septate uterus Journal of contemporary brachytherapy
Platta CS, Wallace C, Gondi V, Das R, Straub M, Al-Niaimi A, Applegate G, Bradley KA
2014 Mar;6(1):76-81. doi: 10.5114/jcb.2014.40768. Epub 2014 Feb 19.
-
More
PURPOSE: To describe an approach to cervical brachytherapy in a patient with congenital septate uterus and locally advanced cervical carcinoma.
MATERIAL AND METHODS: The patient is a 34-year-old female with septate uterus presenting with pelvic pain. Workup demonstrated a stage IIB cervical adenocarcinoma with imaging evidence of an involved right external iliac lymph node. The patient received whole pelvic radiation, with concurrent weekly cisplatin (40 mg/m(2)), to a dose of 45 Gy in 25 fractions followed by a parametrial boost of 5.4 Gy and an additional nodal boost of 9 Gy.
RESULTS: The patient was initiated on cervical brachytherapy following fraction 23 of pelvic radiation. To conform to her septated uterus, a Rotte-Y tandem was used. Additionally, 2 CT-compatible ovoids were placed in the vaginal apex to enhance dose distribution and coverage of the target volume. Each fraction of brachytherapy was performed with CT-based planning. A high-risk clinical target volume (HR-CTV) and normal structures were defined and constrained per American Brachytherapy Society (ABS) and Groupe Européen de Curiethérapie/European Society for Therapeutic Radiology and Oncology (GEC-ESTRO) guidelines. The brachytherapy dose was 27.5 Gy in 5 fractions of 5.5 Gy each, prescribed to the HR-CTV.
CONCLUSIONS: Herein, we report the first documented case of cervical brachytherapy in a patient with septate uterus and locally advanced cervical carcinoma. Using CT-guided planning, in conjunction with the ABS and GEC-ESTRO guidelines, the patient was effectively treated with adapted cervical brachytherapy, meeting criteria for HR-CTV coverage and normal tissue tolerances.
PMID:24790625 | PMC:PMC4003424 | DOI:10.5114/jcb.2014.40768
View details for PubMedID 24790625
-
More
-
Predictive factors of recurrence following adjuvant vaginal cuff brachytherapy alone for stage I endometrial cancer Gynecologic oncology
Dunn EF, Geye H, Platta CS, Gondi V, Rose S, Bradley KA, Anderson BM
2014 Jun;133(3):494-8. doi: 10.1016/j.ygyno.2014.03.554. Epub 2014 Mar 20.
-
More
PURPOSE: The purpose of this study is to identify risk factors for recurrence in a cohort of stage I endometrial cancer patients treated with vaginal cuff brachytherapy at a single academic institution.
METHODS AND MATERIALS: From 1989 to 2011, 424 patients with stage I endometrial cancer underwent total hysterectomy and bilateral salpingo-oophorectomy, with or without lymphadenectomy (LND), followed by high-dose-rate vaginal cuff brachytherapy (VCB) to patients felt to be high or intermediate risk FIGO stage IA and IB disease. Covariates included: 2009 FIGO stage, age, grade, histology, presence of lymphovascular space invasion, LND, and receipt of chemotherapy.
RESULTS: With a median follow-up of 3.7years, the 5 and 10-year disease free survival were 98.4% and 95.9%, respectively. A total of 30 patients developed recurrence, with the predominant pattern of isolated distant recurrence (57.0%). On multivariate analysis, grade 3 (p=0.039) and LND (p=0.048) independently predicted of increased recurrence risk. χ(2) analysis suggested that higher-risk patients were selected for LND, with significant differences in age, stage, and grade noted between cohorts. Distant metastatic rate was significantly higher for patients who qualified for GOG 0249 at 23.1% (95% CI 10.7-35.5%) compared to those who did not at 6.8% (95% CI 1.8-11.8%, p<0.001).
CONCLUSION: Overall disease-free survival for this cohort of patients was >95% at 10years. Univariate analysis confirmed previously identified risk factors as predictors for recurrence. Multivariate analysis found that grade 3 and LND correlated with risk for recurrence. Of those that did recur, the initial site of relapse included distant metastasis in most cases.
PMID:24657301 | DOI:10.1016/j.ygyno.2014.03.554
View details for PubMedID 24657301
-
More
-
Radiation oncology residency selection: a targeted assessment of factor importance among fourth-year medical students International journal of radiation oncology, biology, physics
Brower JV, Mohindra P, Bradley KA, Golden DW
2014 Mar 15;88(4):967-8. doi: 10.1016/j.ijrobp.2013.12.020.
-
Successful management of female urethral carcinoma with radiation therapy and concurrent chemotherapy Gynecologic oncology case reports
Magnuson WJ, Bradley K, Shaves M
2011 Nov 4;2(1):1-3. doi: 10.1016/j.gynor.2011.10.006. eCollection 2011.
-
More
► Successful treatment of locally advanced urethral carcinoma with chemoradiation as evidenced by patients alive NED at 90 and 47 months. ► 45 Gy of external beam RT followed by 15-25 Gy of interstitial brachytherapy. ► Concurrent chemotherapy with 5-fluorouracil and cisplatin.
PMID:24371597 | PMC:PMC3860990 | DOI:10.1016/j.gynor.2011.10.006
View details for PubMedID 24371597
-
More
-
Adjuvant and definitive radiation therapy for primary carcinoma of the vagina using brachytherapy and external beam radiation therapy Journal of contemporary brachytherapy
Platta CS, Anderson B, Geye H, Das R, Straub M, Bradley K
2013 Jun;5(2):76-82. doi: 10.5114/jcb.2013.36177. Epub 2013 Jun 28.
-
More
PURPOSE: To report the outcomes of patients receiving vaginal brachytherapy and/or external beam radiation therapy (EBRT) for primary vaginal cancer.
MATERIAL AND METHODS: Between 1983 and 2009, 63 patients received brachytherapy and/or EBRT for primary tumors of the vagina at a single tertiary center. Patient data was collected via chart review. The Kaplan-Meier method was used to calculate actuarial pelvic local control (LC), disease-free survival (DFS), overall survival (OS), and severe late toxicity rates. Acute and late toxicities were scored according to the Common Terminology Criteria for Adverse Events version 3 (CTCAE v3.0).
RESULTS: Median follow up was 44.2 months. Patients with early stage disease (stages I and II) had significantly improved 5-year OS when compared to patients with locally advanced disease (stages III and IVA) (73.3 vs. 34.4%, p = 0.032). Patients with greater than 1/3 vaginal involvement had significantly worse prognosis than patients with tumors involving 1/3 or less of the vagina, with the later having superior DFS (84.0 vs. 52.4%, p = 0.007) and LC (86.9 vs. 60.4%, p = 0.018) at 5-years. Age, histology, and brachytherapy technique did not impact treatment outcomes. The 5-year actuarial grade 3 or higher toxicity rate was 23.1% (95% CI: 10.6-35.6%). Concurrent chemotherapy had no impact on outcomes or toxicity in this analysis.
CONCLUSIONS: Success of treatment for vaginal cancer depends primarily on disease stage, but other contributing factors such as extent of vaginal involvement and tumor location significantly impact outcomes. Treatment of vaginal cancer with primary radiotherapy yields acceptable results with reasonable toxicity rates. Management of this rare malignancy requires a multidisciplinary approach to appropriately optimize therapy.
PMID:23878551 | PMC:PMC3708150 | DOI:10.5114/jcb.2013.36177
View details for PubMedID 23878551
-
More
-
Effects of treatment duration during concomitant chemoradiation therapy for cervical cancer International journal of radiation oncology, biology, physics
Shaverdian N, Gondi V, Sklenar KL, Dunn EF, Petereit DG, Straub MR, Bradley KA
2013 Jul 1;86(3):562-8. doi: 10.1016/j.ijrobp.2013.01.037. Epub 2013 Apr 2.
-
More
PURPOSE: To determine whether extended treatment duration (TD) impacts in-field relapse and survival in the setting of concomitant chemoradiation therapy (CRT) for cervical cancer.
METHODS AND MATERIALS: A total of 480 consecutive cervical cancer patients treated with radiation therapy (RT) alone or concomitant CRT for curative intent were retrospectively analyzed. Relapse was defined as in-field with respect to external beam radiation therapy fields. The effects of TD on in-field relapse, disease-free survival (DFS), and overall survival (OS) rates were assessed continuously and categorically within the separate RT and CRT cohorts. Covariates included age, histology, stage, and cumulative dose to point A. In-field relapse, DFS, and OS rates were estimated with Kaplan-Meier analysis; comparisons used log-rank statistic. Multivariate analysis used the Cox proportional hazards model.
RESULTS: A total of 372 patients (RT n=206, CRT n=166) were evaluable, with a median follow-up for relapse-free patients of 4.2 years (RT 4.4 years, CRT 4.2 years; P=.807). Treatment duration was longer in the RT cohort (median 55 days; range 35-99 days) versus the CRT cohort (median 51 days; range 35-92 days) (P=.001). In the RT cohort, TD ≥62 days trended to significance for predicting inferior DFS (hazard ratio 1.42, 95% confidence interval 0.86-1.98, P=.086). However, in the CRT cohort, TD assessed continuously or categorically across multiple cutoff thresholds did not predict for in-field relapse, DFS, or OS.
CONCLUSION: With RT alone, extended TD ≥62 days may adversely impact treatment efficacy. With the addition of concomitant chemotherapy to RT, however, extended TD has no effect on treatment efficacy.
PMID:23561652 | DOI:10.1016/j.ijrobp.2013.01.037
View details for PubMedID 23561652
-
More
-
Motexafin-gadolinium and involved field radiation therapy for intrinsic pontine glioma of childhood: a children's oncology group phase 2 study International journal of radiation oncology, biology, physics
Bradley KA, Zhou T, McNall-Knapp RY, Jakacki RI, Levy AS, Vezina G, Pollack IF
2013 Jan 1;85(1):e55-60. doi: 10.1016/j.ijrobp.2012.09.004. Epub 2012 Oct 22.
-
More
PURPOSE: To evaluate the effects on 1-year event-free survival (EFS) and overall survival (OS) of combining motexafin and gadolinium (MGd), a potent radiosensitizer, with daily fractionated radiation therapy in children with newly diagnosed intrinsic pontine gliomas.
METHODS AND MATERIALS: Patients with newly diagnosed intrinsic pontine glioma were treated with MGd daily for 5 consecutive days each week, for a total of 30 doses. Patients received a 5- to 10-min intravenous bolus of MGd, 4.4 mg/kg/day, given 2 to 5 h prior to standard dose irradiation. Radiation therapy was administered at a daily dose of 1.8 Gy for 30 treatments over 6 weeks. The total dose was 54 Gy.
RESULTS: Sixty eligible children received MGd daily, concurrent with 6 weeks of radiation therapy. The estimated 1-year EFS was 18%±5%, and the estimated 1-year OS was 53%±6.5%. The most common grade 3 to 4 toxicities were lymphopenia, transient elevation of liver transaminases, and hypertension.
CONCLUSIONS: Compared to historical controls, the addition of MGd to a standard 6-week course of radiation did not improve the survival of pediatric patients with newly diagnosed intrinsic pontine gliomas.
PMID:23092726 | PMC:PMC3529324 | DOI:10.1016/j.ijrobp.2012.09.004
View details for PubMedID 23092726
-
More
-
Severe late toxicities following concomitant chemoradiotherapy compared to radiotherapy alone in cervical cancer: an inter-era analysis International journal of radiation oncology, biology, physics
Gondi V, Bentzen SM, Sklenar KL, Dunn EF, Petereit DG, Tannehill SP, Straub M, Bradley KA
2012 Nov 15;84(4):973-82. doi: 10.1016/j.ijrobp.2012.01.064. Epub 2012 Aug 14.
-
More
PURPOSE: To compare rates of severe late toxicities following concomitant chemoradiotherapy and radiotherapy alone for cervical cancer.
METHODS AND MATERIALS: Patients with cervical cancer were treated at a single institution with radiotherapy alone or concomitant chemoradiotherapy for curative intent. Severe late toxicity was defined as grade≥3 vaginal, urologic, or gastrointestinal toxicity or any pelvic fracture, using Common Terminology Criteria for Adverse Events version 4.0 (CTCAE), occurring ≥6 months from treatment completion and predating any salvage therapy. Severe late toxicity rates were compared after adjusting for pertinent covariates.
RESULTS: At 3 years, probability of vaginal severe late toxicity was 20.2% for radiotherapy alone and 35.1% for concomitant chemoradiotherapy (P=.026). At 3 years, probability of skeletal severe late toxicity was 1.6% for radiotherapy alone and 7.5% for concomitant chemoradiotherapy (P=.010). After adjustment for case mix, concomitant chemoradiotherapy was associated with higher vaginal (hazard ratio [HR] 3.0, 95% confidence interval [CI], 1.7-5.2, P<.001), and skeletal (HR 7.0, 95% CI 1.4-34.1, P=.016) severe late toxicity. Compared to high dilator compliance, moderate (HR 3.6, 95% CI 2.0-6.5, P<.001) and poor (HR 8.5, 95% CI 4.3-16.9, P<.001) dilator compliance was associated with higher vaginal severe late toxicity. Age>50 was associated with higher vaginal (HR 1.8, 95% CI 1.1-3.0, P=.013) and skeletal (HR 5.7, 95% CI 1.2-27.0, P=.028) severe late toxicity. Concomitant chemoradiotherapy was not associated with higher gastrointestinal (P=.886) or urologic (unadjusted, P=.053; adjusted, P=.063) severe late toxicity.
CONCLUSION: Compared to radiotherapy alone, concomitant chemoradiotherapy is associated with higher rates of severe vaginal and skeletal late toxicities. Other predictive factors include dilator compliance for severe vaginal late toxicity and age for severe vaginal and skeletal late toxicities.
PMID:22898381 | PMC:PMC3706199 | DOI:10.1016/j.ijrobp.2012.01.064
View details for PubMedID 22898381
-
More
-
Patterns of pain and distress during high-dose-rate intracavity brachytherapy for cervical cancer The journal of supportive oncology
Kwekkeboom KL, Dendaas NR, Straub M, Bradley KA
2009 May-Jun;7(3):108-14.
-
More
Over the past decade, outpatient high-dose-rate (HDR) brachytherapy has become increasingly common in the treatment of many women with cervical cancer. In our study, we explored women's experiences of pain and distress over a series of five HDR brachytherapy procedures given for cervical cancer. Seventeen patients receiving HDR cervical brachytherapy with conscious sedation for stages I-III cervical cancer completed ratings of pain intensity and distress and a measure of physical and emotional discomfort with each procedure. The majority of women reported worst pain in the mild to moderate range and similar ratings of worst distress across the series of procedures. The most physically uncomfortable aspect of treatment was removal of the instruments after the procedure, when sedatives had worn off. The most emotionally uncomfortable aspect was worry about the effects of treatment. A subset of women reported having recalled pain from previous procedures, despite the use of conscious sedation medications. Those women who recalled having had pain rated their worst pain during the procedure higher than women who did not recall having had pain. For most patients, HDR brachytherapy delivered with conscious sedation is well tolerated with only mild pain and distress. However, a small number of patients may experience more significant symptoms and may require additional medical and psychosocial support.
PMID:19507459
View details for PubMedID 19507459
-
More
-
The impact of hybrid PET-CT scan on overall oncologic management, with a focus on radiotherapy planning: a prospective, blinded study Technology in cancer research & treatment
Kruser TJ, Bradley KA, Bentzen SM, Anderson BM, Gondi V, Khuntia D, Perlman SB, Tome WA, Chappell RJ, Walker WL, Mehta MP
2009 Apr;8(2):149-58. doi: 10.1177/153303460900800208.
-
More
Functional imaging using fluorodeoxyglucose positron-emission tomography (FDG-PET) has been increasing incorporated into radiotherapy planning in conjunction with computed tomography (CT). Hybrid FDG-PET/CT scanners allow these images to be obtained in very close temporal proximity without the need for repositioning patients, thereby minimizing imprecision when overlying these images. To prospectively examine the impact of hybrid PET/CT imaging on overall oncologic impact, with a focus on radiotherapy planning, we performed a prospective, blinded trial in 111 patients. Patients with lung cancer (n=38), head-and-neck squamous cell carcinoma (n=23), breast (n=8), cervix (n=15), esophageal (n=9), and lymphoma (n=18) underwent hybrid PET/CT imaging at the time of radiation therapy planning. A physician blinded to the PET dataset designed a treatment plan using all clinical information and the CT dataset. The treating physician subsequently designed a second treatment plan using the hybrid PET/CT dataset. The two treatment plans were compared to determine if a major alteration in overall oncologic management occured. In patients receiving potentially curative radiotherapy the concordance between CT-based and PET/CT-based GTVs was quantified using an index of conformality (CI). In 76/111 (68%) of patients, the PET/CT data resulted in a change in one or more of the following: GTV volume, regional/local extension, prescribed dose, or treatment modality selection. In 35 of these 76 cases (46%; 31.5% of the entire cohort) the change resulted in a major alteration in the oncologic management (dose, field design, or modality change). Thus, nearly a third of all cases had a major alteration in oncologic management as a result of the PET/CT data, and 29 of 105 patients (27.6%) who underwent potentially curative radiotherapy had major alterations in either dose or field design. Hybrid PET/CT imaging at the time of treatment planning may be highly informative and an economical manner in which to obtain PET imaging, with the dual goals of staging and treatment planning.
PMID:19334796 | DOI:10.1177/153303460900800208
View details for PubMedID 19334796
-
More
-
Motexafin gadolinium and involved field radiation therapy for intrinsic pontine glioma of childhood: a Children's Oncology Group phase I study Neuro-oncology
Bradley KA, Pollack IF, Reid JM, Adamson PC, Ames MM, Vezina G, Blaney S, Ivy P, Zhou T, Krailo M, Reaman G, Mehta MP, Group CO
2008 Oct;10(5):752-8. doi: 10.1215/15228517-2008-043. Epub 2008 Aug 20.
-
More
The purpose of this study was to determine the dose-limiting toxicities, maximum tolerated dose, pharmacokinetics, and intratumor and brain distribution of motexafin gadolinium (MGd) with involved field radiation therapy in children with newly diagnosed intrinsic pontine gliomas. MGd was administered as a 5-min intravenous bolus 2-5 h prior to standard radiation. The starting dose was 1.7 mg/kg. After first establishing that 5 doses/week for 6 weeks was tolerable, the dose of MGd was escalated until dose-limiting toxicity was reached. Radiation therapy was administered to 54 Gy in 30 once-daily fractions. Forty-four children received MGd at doses of 1.7 to 9.2 mg/kg daily prior to radiation therapy for 6 weeks. The maximum tolerated dose was 4.4 mg/kg. The primary dose-limiting toxicities were grade 3 and 4 hypertension and elevations in serum transaminases. Median elimination half-life and clearance values were 6.6 h and 25.4 ml/kg/h, respectively. The estimated median survival was 313 days (95% confidence interval, 248-389 days). The maximum tolerated dose of MGd and the recommended phase II dose was 4.4 mg/kg when administered as a daily intravenous bolus in conjunction with 6 weeks of involved field radiation therapy for pediatric intrinsic pontine gliomas.
PMID:18715950 | PMC:PMC2666252 | DOI:10.1215/15228517-2008-043
View details for PubMedID 18715950
-
More
-
The effect of laparoscopic guidance on gynecologic interstitial brachytherapy Journal of minimally invasive gynecology
Engle DB, Bradley KA, Chappell RJ, Conner JP, Hartenbach EM, Kushner DM
2008 Sep-Oct;15(5):541-6. doi: 10.1016/j.jmig.2008.06.001. Epub 2008 Jul 26.
-
More
STUDY OBJECTIVE: To compare laparoscopic-assisted interstitial brachytherapy (LAIB) with traditional interstitial brachytherapy (TrIB) in the treatment of gynecologic malignancies.
DESIGN: Retrospective review (Canadian Task Force classification II-3).
SETTING: University hospital.
PATIENTS: A total of 42 women undergoing interstitial brachytherapy for a gynecologic malignancy.
INTERVENTIONS: Interstitial brachytherapy by traditional method versus laparoscopic guidance.
MEASUREMENTS AND MAIN RESULTS: In all, 42 women underwent interstitial brachytherapy with a mean follow-up of 24 months. In all, 28 patients underwent TrIB and 14 underwent LAIB. The mean operating department time was 177 minutes for LAIB and 91 minutes for TrIB (p<.001). No intraoperative complications existed in either group. Of the 14 patients undergoing LAIB, 2 (14%) had carcinomatosis, and the brachytherapy was aborted. Of patients who proceeded with LAIB, 64% had clinically significant pelvic adhesions necessitating lysis of adhesions. Mean radiation doses were similar for both external beam (LAIB=54 Gy, TrIB=50 Gy; p=.12) and brachytherapy (LAIB=29 Gy, TrIB=30 Gy; p=.8). No difference existed in the mean follow-up between groups (p=.7). In regard to long-term grade 3/4 radiation toxicity, 1 (10%) patient undergoing LAIB had a rectovaginal fistula. Six (27%) patients (p=.39; 95% CI 9%-43%) undergoing TrIB experienced high-grade toxicity, including 2 rectovaginal fistulas, 1 rectal stricture, 1 necrotizing fasciitis, 1 urinary incontinence, and 1 soft-tissue necrosis.
CONCLUSION: The LAIB procedure appears safe, but substantially increases operating department time. No significant decrease in late high-grade toxicities were detected in comparison with TrIB. The LAIB procedure allows for both lysis of adhesions and identification of unknown carcinomatosis.
PMID:18657479 | DOI:10.1016/j.jmig.2008.06.001
View details for PubMedID 18657479
-
More
-
Impact of hybrid fluorodeoxyglucose positron-emission tomography/computed tomography on radiotherapy planning in esophageal and non-small-cell lung cancer International journal of radiation oncology, biology, physics
Gondi V, Bradley K, Mehta M, Howard A, Khuntia D, Ritter M, Tomé W
2007 Jan 1;67(1):187-95. doi: 10.1016/j.ijrobp.2006.09.033.
-
More
PURPOSE: The aim of this study was to investigate the impact of a hybrid fluorodeoxyglucose positron-emission tomography/computed tomography (FDG-PET/CT) scanner in radiotherapy planning for esophageal and non-small-cell lung cancer (NSCLC).
METHODS AND MATERIALS: A total of 30 patients (16 with esophageal cancer, 14 with NSCLC) underwent an FDG-PET/CT for radiotherapy planning purposes. Noncontrast total-body spiral CT scans were obtained first, followed immediately by FDG-PET imaging which was automatically co-registered to the CT scan. A physician not involved in the patients' original treatment planning designed a gross tumor volume (GTV) based first on the CT dataset alone, while blinded to the FDG-PET dataset. Afterward, the physician designed a GTV based on the fused PET/CT dataset. To standardize PET GTV margin definition, background liver PET activity was standardized in all images. The CT-based and PET/CT-based GTVs were then quantitatively compared by way of an index of conformality, which is the ratio of the intersection of the two GTVs to their union.
RESULTS: The mean index of conformality was 0.44 (range, 0.00-0.70) for patients with NSCLC and 0.46 (range, 0.13-0.80) for patients with esophageal cancer. In 10 of the 16 (62.5%) esophageal cancer patients, and in 12 of the 14 (85.7%) NSCLC patients, the addition of the FDG-PET data led to the definition of a smaller GTV.
CONCLUSION: The incorporation of a hybrid FDG-PET/CT scanner had an impact on the radiotherapy planning of esophageal cancer and NSCLC. In future studies, we recommend adoption of a conformality index for a more comprehensive comparison of newer treatment planning imaging modalities to conventional options.
PMID:17189070 | DOI:10.1016/j.ijrobp.2006.09.033
View details for PubMedID 17189070
-
More
-
Radiation therapy for gynecologic malignancies Hematology/oncology clinics of North America
Bradley KA, Petereit DG
2006 Apr;20(2):347-61. doi: 10.1016/j.hoc.2006.01.019.
-
More
In the last century, radiation has been successfully used as primary and adjuvant treatment in the management of gynecologic malignancies. It is anticipated that radiation will continue as an integral component in the treatment of cervical,endometrial, vulvar, and vaginal carcinoma. Current efforts are directed at im-proving control rates while minimizing treatment-related toxicities through the use of more conformal external beam radiotherapy techniques, refinement of brachytherapy techniques, and the integration of chemotherapy.
PMID:16730298 | DOI:10.1016/j.hoc.2006.01.019
View details for PubMedID 16730298
-
More
-
Quality assurance of treatment plans for interstitial and intracavitary high-dose-rate brachytherapy Brachytherapy
Das RK, Bradley KA, Nelson IA, Patel R, Thomadsen BR
2006 Jan-Mar;5(1):56-60. doi: 10.1016/j.brachy.2005.11.002.
-
More
PURPOSE: Quality assurance for complex high-dose-rate (HDR) treatment planning has always been a challenge to the physics community because of the time constraint between HDR planning and the delivery of the treatment. This study proposes an efficient, precise, and easy method for checking the complex computer calculation.
METHODS AND MATERIALS: Posttreatment, three-dimensional dose-volume study was performed for 98 patients with 128 new treatment plans along with 30 library plans. Volumes covered by the 100% isodose line, source activity (Ci), total dwell time (s), and the prescription dose (100%) were recorded. Variation of R(V) defined as (irradiated time x activity/elongation factor x prescribed dose) with volume was studied for different catheter systems.
RESULTS: Parametric fit of R(V) with volume for three different systems that cover most of the interstitial and intracavitary brachytherapy implants agrees within +/-6%.
CONCLUSIONS: The excellent agreement of R(V) derived from this simplistic point source model with three-dimensional dose calculations for individual HDR treatment plans clearly establishes that for an implant with known number of catheters, the time needed to deliver a prescribed dose to a given prescription volume can be easily predicted.
PMID:16563998 | DOI:10.1016/j.brachy.2005.11.002
View details for PubMedID 16563998
-
More
-
Linear accelerator radiosurgery for trigeminal neuralgia Neurosurgery
Richards GM, Bradley KA, Tomé WA, Bentzen SM, Resnick DK, Mehta MP
2005 Dec;57(6):1193-200; discussion 1193-200. doi: 10.1227/01.neu.0000186015.01179.70.
-
More
OBJECTIVE: To report the clinical outcomes following treatment of trigeminal neuralgia with linear accelerator-based radiosurgery.
METHODS: Twenty-eight patients with medication refractory idiopathic trigeminal neuralgia were treated with a single fraction of 80 Gy to the trigeminal nerve root. For treatment delivery, a 4-mm collimator and a 7-arc technique were delivered using a stereotactic floor stand system with an isocenter stability of 0.2 +/- 0.1 mm to minimize dose to the brainstem. Treatment delivery time was approximately 55 minutes.
RESULTS: With a median follow-up of 12 months (range, 1-40 mo), 57% of patients achieved complete pain relief and 75% (exact 95% confidence interval, 55 to 89%) had their pain reduced to 3 or less on a 10-point pain scale. Median time to pain relief was 1 month. Four patients did not respond to treatment. The actuarial mean time to pain recurrence in responders was 14 months, and the actuarial mean response duration in major to complete responders was 16 months. Women had significantly longer mean time to pain recurrence than men (16 versus 7 months; P = 0.05). Three patients reported new mild facial numbness after radiosurgery and one patient developed neurotrophic keratopathy.
CONCLUSION: Linear accelerator-based radiosurgery for medication refractory trigeminal neuralgia provides effective pain relief with a low complication rate.
PMID:16331167 | DOI:10.1227/01.neu.0000186015.01179.70
View details for PubMedID 16331167
-
More
-
Radiation therapy for leptomeningeal cancer Cancer treatment and research
Mehta M, Bradley K
2005;125:147-58. doi: 10.1007/0-387-24199-x_9.
-
More
Radiotherapy has multiple roles in the treatment of leptomeningeal cancer. While it is uncommon for patients to experience regression of neurologic deficits due to leptomeningeal cancer, focal radiotherapy often provides significant palliation of pain, increased intracranial pressure and other focal symptoms. Focal radiotherapy may also be used to eliminate blockages of cerebrospinal fluid (CSF) and allow for safe administration of intrathecal chemotherapy. Craniospinal irradiation (CSI) is most often used as prophylaxis for patients at high risk of leptomeningeal tumor dissemination, but may result in symptom palliation and prolonged disease control for patients with active leptomeningeal tumor.
PMID:16211888 | DOI:10.1007/0-387-24199-x_9
View details for PubMedID 16211888
-
More
-
Management of brain metastases Seminars in oncology
Bradley KA, Mehta MP
2004 Oct;31(5):693-701. doi: 10.1053/j.seminoncol.2004.07.012.
-
More
Patients with brain metastases have a generally poor outcome with a median survival after diagnosis of approximately 4 months. Management of brain metastases involves symptomatic treatment and definitive therapy, with the goal of stabilizing and improving neurologic function and survival. Traditional and novel therapies, including whole-brain radiation therapy (WBRT), surgery, radiosurgery, radiosensitizers, and chemotherapy are reviewed. The results of important clinical trials are discussed. In addition, current controversies in the management of brain metastases, such as the choice of surgery or radiosurgery for resectable lesions and the possible avoidance of (WBRT), are highlighted.
PMID:15497123 | DOI:10.1053/j.seminoncol.2004.07.012
View details for PubMedID 15497123
-
More
-
Megavoltage computed tomography imaging: a potential tool to guide and improve the delivery of thoracic radiation therapy Clinical lung cancer
Welsh JS, Bradley K, Ruchala KJ, Mackie TR, Mañon R, Patel R, Wiederholt P, Lock M, Hui S, Mehta MP
2004 Mar;5(5):303-6. doi: 10.3816/CLC.2004.n.010.
-
More
Helical tomotherapy is an innovative means of delivering intensity-modulated radiation therapy (IMRT) using a device that merges features of a linear accelerator and a helical computed tomography (CT) scanner. The tomotherapy unit can generate CT images from the megavoltage radiation it uses for treatment as often as needed during a course of radiation therapy. These megavoltage CT (MVCT) images offer verification of patient position prior to and potentially during radiation therapy, and provide considerably more anatomical detail than the conventional radiation therapy port films used for patient set-up verification. Also, MVCT imaging may enable reconstruction of the radiation dose delivered, thereby providing unprecedented verification of the actual treatment. These key features of helical tomotherapy distinguish it from other IMRT approaches. We report results from a pilot feasibility trial of 10 patients with non-small-cell lung cancer (NSCLC) on whom we obtained MVCT images using a prototype helical tomotherapy system. All patients underwent conventional CT imaging for radiation therapy treatment planning. Specific aims were to subjectively compare MVCT and conventional CT images and then to objectively compare the 2 modalities by contouring tumors and performing a volumetric comparison. Seven patients had disease located primarily in the lung parenchyma, 2 primarily in the mediastinum, and 1 in both. When evaluated by location, all 7 patients with lesions primarily in the lung parenchyma had subjectively high-quality MVCT images. Objectively, the volumetric agreement between conventional and MVCT for parenchymal lesions was excellent in 5 of the 7 patients. Megavoltage CT imaging via the helical tomotherapy prototype provided adequate information for use in verification of patient position and dose reconstruction for lesions within the pulmonary parenchyma, but presently appears suboptimal for primarily mediastinal disease. Further studies are ongoing to optimize MVCT imaging and better define its utility in patients with NSCLC.
PMID:15086969 | DOI:10.3816/CLC.2004.n.010
View details for PubMedID 15086969
-
More
Contact Information
Kristin Bradley, MD
600 Highland Avenue,Madison, WI 53792
