I am an associate professor and director of Clinical Physics in the Department of Human Oncology. As a medical physicist in radiation therapy, my role is to ensure the safe, effective and accurate delivery of radiation to our patients as well as the protection of the general public from our treatment activities. I am the lead physicist for our stereotactic radiosurgery (SRS) program. Through these efforts, I spend most of my time clinically working with patients requiring treatment for primary or metastatic intracranial disease, ensuring the most accurate treatments possible. SRS treatments include the smallest and highest dose-per-fraction treatments delivered anywhere in radiation therapy, so my focus is on highly conformal delivery and planning techniques.
My research interests include methods to improve the accuracy of treatment alignment and delivery strategies, with the goal of reducing the total spatial uncertainty in SRS treatments, and to develop new treatment planning strategies that result in very robust yet efficient treatment plans for SRS patients. I also work with graduate students and faculty in medical physics on research efforts to more precisely measure doses from modern treatment systems.
I also serve as the director of our Radiation Oncology Physics Residency Program, overseeing the day-to-day efforts of our residents and setting the vision and organizational structure of our training program. Working with young medical physicists during their transition from graduate student to independent clinical physicist is a highly rewarding experience, and my ultimate goal is to create a learning environment where our graduating residents can positively impact the radiation oncology patient condition by enabling the highest quality of care everywhere they go.
Education
Residency, University of Michigan, Clinical Medical Physics (2014)
PhD, University of Chicago, Medical Physics (2012)
BS, University of Wisconsin–Madison, Applied Mathematics, Engineering and Physics (2007)
Academic Appointments
Associate Professor (CHS), Human Oncology (2021)
Assistant Professor (CHS), Human Oncology (2015)
Assistant Researcher, Human Oncology (2014)
Selected Honors and Awards
Clinical Physics Educator Award (2019)
Good Catch Great Care Award, Human Oncology (2019)
University of Chicago Biological Sciences Division Outstanding Performance Award in the Field of Medical Physics (2012)
First Place, Young Investigator Session, Midwest Chapter AAPM Spring Meeting (2011)
University of Chicago Doolittle-Harrison Fellowship (2011)
University of Chicago Graduate Program in Medical Physics, Lawrence Lanzl Award for Exceptional Research Ability in Medical Physics (2010)
First Place, Young Investigator Session, North Central Chapter AAPM Fall Meeting (2010)
Paul C. Hodges Research Award in Radiology (2009–2010)
Phi Beta Kappa, University of Wisconsin–Madison (2007)
AAPM Summer Undergraduate Fellowship Award (2006)
Radtke Award for Undergraduate Academic Achievement in Physics (2004)
Dean’s List, University of Wisconsin–Madison (2003–2007)
National Merit Scholar (2003–2007)
Boards, Advisory Committees and Professional Organizations
Presidential Chain, North Central Chapter of the American Association of Physicists in Medicine (2018-2020)
Reviewer for multiple journals and annual meetings (including Medical Physics, Medical Dosimetry, Int J Rad Onc Biol Phys, AAPM Annual Meeting, etc.)
Vice Chair, Journals Business Management Committee, American Association of Physicists in Medicine
Chair, Radiation Oncology Physics Residency Program Oversight Committee, University of Wisconsin–Madison
Chair, Radiation Oncology Physics Residency Program Selection Committee, University of Wisconsin–Madison
Research Focus
Brain, Spine
Dr. Zacariah Labby is the lead physicist for the department’s Varian TrueBeam platform and the lead physicist for the department’s stereotactic radiosurgery (SRS) program. His research interests include methods to improve the accuracy of treatment alignment and delivery strategies.
Improving the precision and accuracy of what we do will allow us to help more patients, more effectively than ever before.
In radiation therapy, we know that dose delivered through small fields must be measured differently, but how, exactly? We know that modern treatment systems can compensate for spatial inaccuracies, but will such strategies always work? I’m interested in finding and eradicating imprecision in the technical aspects of radiation therapy.
Treatment Planning Strategies for Stereotactic Radiosurgery
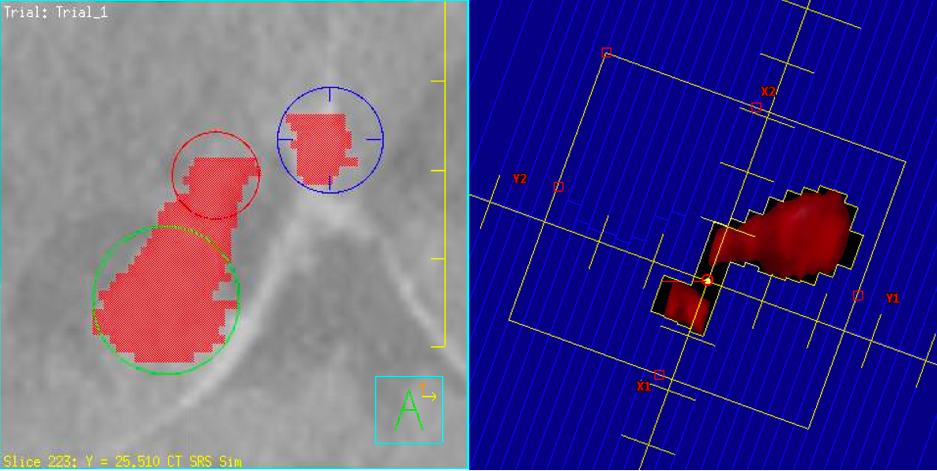
For intracranial radiosurgery treatments, we seek conformal high-dose radiation dose distributions with exceptionally sharp fall-off of the dose outside the treatment volume. Depending on the exact size, shape and location of the target volume, we have access to different treatment planning approaches to achieve these goals. We could treat the target with multiple “shots” of radiation built up from spherical doses with circular conical collimators, or we could treat the target with customized multi-leaf collimator sequences. Sometimes we wish to center the radiation beams exactly in the center of one target, and sometimes we wish to treat multiple targets all with the same localization. We’re working to quantify the exact trade-offs between various treatment planning strategies to better decide the optimal strategy for every unique patient.
Patient Plan-Specific Detector Corrections for Accurate Radiation Measurements
It is well known in radiation physics that ionization chambers respond differently to small fields of radiation (compared to larger fields) due to spectral response characteristics and variable perturbation effects. What is less well known is the magnitude of these effects for any particular patient plan, or for a patient plan characterized by modulation indices, etc. We are working with a graduate student in the UW Radiation Calibration Laboratory to better quantify these effects to enable more accurate radiation dose measurements for individual patients and to enable more precise computer modeling of radiation delivery systems.
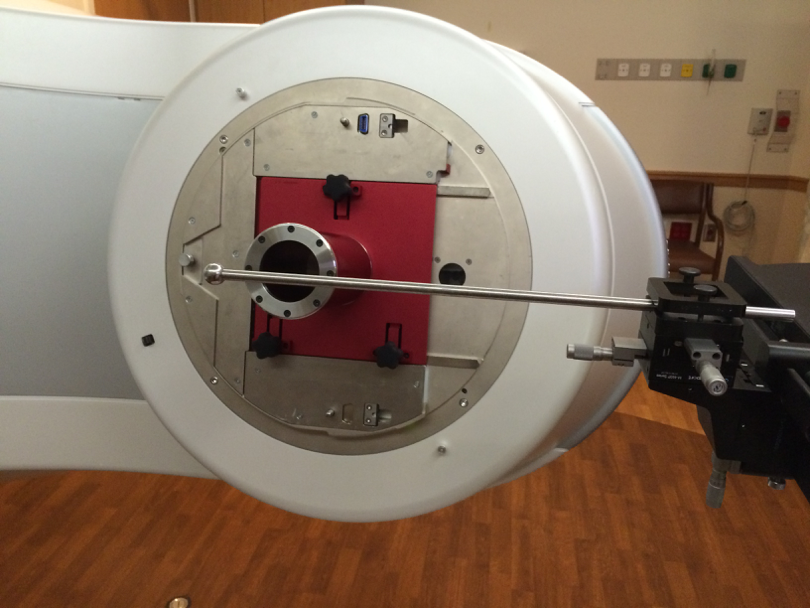
Improving the Mechanical Precision of Radiation Therapy Delivery
I’m especially fascinated with the potential to improve the mechanical precision of radiation therapy treatment delivery through a variety of strategies. I’m working on techniques to better align conical collimators with the delivery system axes and to ensure that alignment is stable over time. I’m working on more complete and more efficient tests to check the accuracy of multi-leaf collimator positioning, down to 0.05 mm or better. I’m also working on active strategies to compensate for mechanical flex and misalignment, with the goal of overall combined mechanical accuracy on the order of 0.2 mm.
-
Portability of IMRT QA between matched linear accelerators Journal of applied clinical medical physics
Barraclough B, Labby ZE, Frigo SP
2024 Oct;25(10):e14492. doi: 10.1002/acm2.14492. Epub 2024 Sep 9.
-
More
PURPOSE: To determine if patient-specific IMRT quality assurance can be measured on any matched treatment delivery system (TDS) for patient treatment delivery on another.
METHODS: Three VMAT plans of varying complexity were created for each available energy for head and neck, SBRT lung, and right chestwall anatomical sites. Each plan was delivered on three matched Varian TrueBeam TDSs to the same Scandidos Delta4 Phantom+ diode array with only energy-specific device calibrations. Dose distributions were corrected for TDS output and then compared to TPS calculations using gamma analysis. Round-robin comparisons between measurements from each TDS were also performed using point-by-point dose difference, median dose difference, and the percent of point dose differences within 2% of the mean metrics.
RESULTS: All plans had more than 95% of points passing a gamma analysis using 3%/3 mm criteria with global normalization and a 20% threshold when comparing measurements to calculations. The tightest gamma analysis criteria where a plan still passed > 95% were similar across delivery systems-within 0.5%/0.5 mm for all but three plan/energy combinations. Median dose deviations in measurement-to-measurement comparisons were within 0.7% and 1.0% for global and local normalization, respectively. More than 90% of the point differences were within 2%.
CONCLUSION: A set of plans spanning available energies and complexity levels were delivered by three matched TDSs. Comparisons to calculations and between measurements showed dose distributions delivered by each TDS using the same DICOM RT-plan file meet tolerances much smaller than typical clinical IMRT QA criteria. This demonstrates each TDS is modeled to a similar accuracy by a common class (shared) beam model. Additionally, it demonstrates that dose distributions from one TDS show small differences in median dose to the others. This is an important validation component of the common beam model approach, allowing for operational improvements in the clinic.
PMID:39250771 | PMC:PMC11466462 | DOI:10.1002/acm2.14492
View details for PubMedID 39250771
-
More
-
Medical Physics ends print Medical physics
Boone JM, Benedict SH, Labby ZE, Armato SG
2023 Oct;50(10):5933-5934. doi: 10.1002/mp.16766.
-
Commissioning an Exradin W2 plastic scintillation detector for clinical use in small radiation fields Journal of applied clinical medical physics
Jacqmin DJ, Miller JR, Barraclough BA, Labby ZE
2022 Aug;23(8):e13728. doi: 10.1002/acm2.13728. Epub 2022 Jul 21.
-
More
PURPOSE: The purpose of this work is to evaluate the Standard Imaging Exradin W2 plastic scintillation detector (W2) for use in the types of fields used for stereotactic radiosurgery.
METHODS: Prior to testing the W2 in small fields, the W2 was evaluated in standard large field conditions to ensure good detector performance. These tests included energy dependence, short-term repeatability, dose-response linearity, angular dependence, temperature dependence, and dose rate dependence. Next, scan settings and calibration of the W2 were optimized to ensure high quality data acquisition. Profiles of small fields shaped by cones and multi-leaf collimator (MLCs) were measured using the W2 and IBA RAZOR diode in a scanning water tank. Output factors for cones (4-17.5 mm) and MLC fields (1, 2, 3 cm) were acquired with both detectors. Finally, the dose at isocenter for seven radiosurgery plans was measured with the W2 detector.
RESULTS: W2 exhibited acceptable warm-up behavior, short-term reproducibility, axial angular dependence, dose-rate linearity, and dose linearity. The detector exhibits a dependence upon energy, polar angle, and temperature. Scanning measurements taken with the W2 and RAZOR were in good agreement, with full-width half-maximum and penumbra widths agreeing to within 0.1 mm. The output factors measured by the W2 and RAZOR exhibited a maximum difference of 1.8%. For the seven point-dose measurements of radiosurgery plans, the W2 agreed well with our treatment planning system with a maximum deviation of 2.2%. The Čerenkov light ratio calibration method did not significantly impact the measurement of relative profiles, output factors, or point dose measurements.
CONCLUSION: The W2 demonstrated dosimetric characteristics that are suitable for radiosurgery field measurements. The detector agreed well with the RAZOR diode for output factors and scanned profiles and showed good agreement with the treatment planning system in measurements of clinical treatment plans.
PMID:35861648 | PMC:PMC9359019 | DOI:10.1002/acm2.13728
View details for PubMedID 35861648
-
More
-
Prospective Study of PET/MRI Tumor Response During Chemoradiotherapy for Patients With Low-risk and Intermediate-risk p16-positive Oropharynx Cancer American journal of clinical oncology
Witek ME, Kimple RJ, Avey GD, Burr AR, Chandereng T, Yu M, Hu R, Wieland AM, Labby ZE, Bruce JY, Brower JV, Hartig GK, Harari PM
2022 May 1;45(5):202-207. doi: 10.1097/COC.0000000000000910. Epub 2022 Apr 12.
-
More
OBJECTIVE: The objective of this study was to examine tumor response with positron emission tomography (PET)/magnetic resonance imaging (MRI) during chemoradiotherapy as a predictor of outcome in patients with p16-positive oropharynx cancer.
MATERIALS AND METHODS: Patients with p16-positive oropharynx cancer were treated with chemoradiotherapy. Low-risk (LR) disease was defined as T1-T3 and N0-2b and ≤10 pack-years and intermediate-risk (IR) disease as T4 or N2c-3 or >10 pack-years. Patients underwent a PET/MRI scan pretreatment and at fraction 10. Change in value of imaging means were analyzed by analysis of variance. K-means clustering with Euclidean distance functions were used for patient clustering. Silhouette width was used to determine the optimal number of clusters. Linear regression was performed on all radiographic metrics using patient and disease characteristics.
RESULTS: Twenty-four patients were enrolled with 7 LR and 11 IR patients available for analysis. Pretreatment imaging characteristics between LR and IR patients were similar. Patients with LR disease exhibited a larger reduction in maximum standardized uptake value (SUV) compared with IR patients (P<0.05). Cluster analysis defined 2 cohorts that exhibited a similar intratreatment response. Cluster 1 contained 7 of 7 LR patients and 8 of 11 IR patients. Cluster 2 contained 3 of 11 IR patients. Cluster 2 exhibited significant differences compared with cluster 1 in the change in primary tumor peak SUV and largest lymph node median SUV.
CONCLUSIONS: We identified that IR p16-positive oropharynx cancers exhibit heterogeneity in their PET/MRI response to chemoradiotherapy. These data support further study of intratreatment imaging response as a potential mechanism to identify patients with IR oropharynx cancer suitable for treatment deintensification.
PMID:35446279 | PMC:PMC9623610 | DOI:10.1097/COC.0000000000000910
View details for PubMedID 35446279
-
More
-
Stereotactic Radiation Therapy for an Arteriovenous Malformation of the Oral Tongue: A Teaching Case Advances in radiation oncology
Merfeld EC, Labby ZE, Miller JR, Burr AR, Wong F, Diamond C, Wieland AR, Aagaard-Kienitz B, Howard SP
2021 Dec 16;7(3):100870. doi: 10.1016/j.adro.2021.100870. eCollection 2022 May-Jun.
-
Diagnosing atmospheric communication of a sealed monitor chamber Journal of applied clinical medical physics
McCaw TJ, Barraclough BA, Belanger M, Besemer A, Dunkerley AP, Labby ZE
2020 Aug;21(8):309-314. doi: 10.1002/acm2.12975. Epub 2020 Jul 10.
-
More
Daily output variations of up to ±2% were observed for a protracted time on a Varian TrueBeam® STx; these output variations were hypothesized to be the result of atmospheric communication of the sealed monitor chamber. Daily changes in output relative to baseline, measured with an ionization chamber array (DQA3) and the amorphous silicon flat panel detector (IDU) on the TrueBeam®, were compared with daily temperature-pressure corrections (PTP ) determined from sensors within the DQA3. Output measurements were performed using a Farmer® ionization chamber over a 5-hour period, during which there was controlled variation in the monitor chamber temperature. The root mean square difference between percentage output change from baseline measured with the DQA3 and IDU was 0.50% over all measurements. Over a 7-month retrospective review of daily changes in output and PTP , weak correlation (R2 = 0.30) was observed between output and PTP for the first 5 months; for the final 2 months, daily output changes were linearly correlated with changes in PTP , with a slope of 0.84 (R2 = 0.89). Ionization measurements corrected for ambient temperature and pressure during controlled heating and cooling of the monitor chamber differed from expected values for a sealed monitor chamber by up to 4.6%, but were consistent with expectation for an air-communicating monitor chamber within uncertainty (1.3%, k = 2). Following replacement of the depressurized monitor chamber, there has been no correlation between daily percentage change in output and PTP (R2 = 0.09). The utility of control charts is demonstrated for earlier identification of changes in the sensitivity of a sealed monitor chamber.
PMID:32648368 | PMC:PMC7484838 | DOI:10.1002/acm2.12975
View details for PubMedID 32648368
-
More
-
On the implementation of the plan-class specific reference field using multidimensional clustering of plan features and alternative strategies for improved dosimetry in modulated clinical linear accelerator treatments Medical physics
Desai VK, Labby ZE, DeWerd LA, Culberson WS
2020 Aug;47(8):3621-3635. doi: 10.1002/mp.14207. Epub 2020 May 18.
-
More
PURPOSE: The plan-class specific reference field concept could theoretically improve the calibration of radiation detectors in a beam environment much closer to clinical deliveries than existing broad beam dosimetry protocols. Due to a lack of quantitative guidelines and representative data, however, the pcsr field concept has not yet been widely implemented. This work utilizes quantitative plan complexity metrics from modulated clinical treatments in order to investigate the establishment of potential plan classes using two different clustering methodologies. The utility of these potential plan clusters is then further explored by analyzing their relevance to actual dosimetric correction factors.
METHODS: Two clinical databases containing several hundred modulated plans originally delivered on two Varian linear accelerators were analyzed using 21 plan complexity metrics. In the first approach, each database's plans were further subdivided into groups based on the anatomic site of treatment and then compared to one another using a series of nonparametric statistical tests. In the second approach, objective clustering algorithms were used to seek potential plan clusters in the multidimensional complexity-metric space. Concurrently, beam- and detector-specific dosimetric corrections for a subset of the modulated clinical plans were determined using Monte Carlo for three different ionization chambers. The distributions of the dosimetric correction factors were compared to the derived plan clusters to see which plan clusters, if any, could help predict the correction factor magnitudes. Ultimately, a simplified volume averaging metric (SVAM) is shown to be much more relevant to the total dosimetric correction factor than the established plan clusters.
RESULTS: Plan groups based on the site of treatment did not show noticeable distinction from one another in the context of the metrics investigated. An objective clustering algorithm was able to discriminate volumetric modulated arc therapy (VMAT) plans from step-and-shoot intensity-modulated radiation therapy plans with an accuracy of 90.8%, but no clusters were found to exist at any level more specific than delivery modality. Monte Carlo determined correction factors for the modulated plans ranged from 0.970 to 1.104, 0.983 to 1.027, and 0.986 to 1.009 for the A12, A1SL, and A26 chambers, respectively, and were highly variable even within the treatment modality plan clusters. The magnitudes of these correction factors were explained almost entirely by volume averaging with SVAM demonstrating positive correlation with all Monte Carlo established total correction factors.
CONCLUSIONS: Plan complexity metrics do provide some quantitative basis for the investigation of plan clusters, but an objective clustering algorithm demonstrated that quantifiable differences could only be found between VMAT and step-and-shoot beams delivered on the same treatment machine. The inherent variability of the Monte Carlo determined correction factors could not be explained solely by the modality of the treatment but were instead almost entirely dependent upon the volume averaging correction, which itself depends on the detector position within the dose distribution, dose gradients, and other factors. Considering the continued difficulty of determining a relevant plan metric to base plan clusters on, case-by-case corrections may instead obviate the need for the pcsr field concept in the future.
PMID:32337734 | DOI:10.1002/mp.14207
View details for PubMedID 32337734
-
More
-
Calculating dose from a 2.5 MV imaging beam using a commercial treatment planning system Journal of applied clinical medical physics
Ferris WS, Culberson WS, Anderson DR, Labby ZE
2019 Dec;20(12):25-35. doi: 10.1002/acm2.12756. Epub 2019 Nov 1.
-
More
Patient dose from 2.5 MV images on the TrueBeam linear accelerator is not easily quantified, primarily because this beam energy is not normally modeled by commercial treatment planning systems. In this work we present the feasibility of using the Eclipse® treatment planning system to model this beam. The Acuros XB and the AAA dose calculation algorithms were tested. Profiles, PDDs, and output factors were measured for the 2.5 MV unflattened imaging beam and used for beam modeling. The algorithms were subsequently verified using MPPG 5.a guidelines. Calculated doses with both algorithms agreed with the measurement data to within the following criteria recommended for conventional therapeutic MV beams: 2% local dose-difference in the high-dose region, 3% global difference in the low-dose region, 3 mm distance to agreement in the penumbra, and a gamma pass rate of >95% for 3%/3 mm criteria. Acuros was able to accurately calculate dose through cork and bone-equivalent heterogeneities. AAA was able to accurately calculate dose through the bone-equivalent heterogeneity but did not pass within the recommended criteria for the cork heterogeneity. For the 2.5 MV imaging beam, both the AAA and Acuros algorithms provide calculated doses that agree with measured results well within the 20% criteria for imaging beams recommended by AAPM TG-180.
PMID:31675460 | PMC:PMC6909176 | DOI:10.1002/acm2.12756
View details for PubMedID 31675460
-
More
-
Impact of adjuvant fractionated stereotactic radiotherapy dose on local control of brain metastases Journal of neuro-oncology
Musunuru HB, Witt JS, Yadav P, Francis DM, Kuczmarska-Haas A, Labby ZE, Bassetti MF, Howard SP, Baschnagel AM
2019 Nov;145(2):385-390. doi: 10.1007/s11060-019-03308-7. Epub 2019 Oct 12.
-
More
PURPOSE: The aim of this study was to determine whether a higher biological effective dose (BED) would result in improved local control in patients treated with fractionated stereotactic radiotherapy (FSRT) for their resected brain metastases.
METHODS: Patients with newly diagnosed brain metastases without previous brain radiotherapy were retrospectively reviewed. Patients underwent surgical resection of at least one brain metastasis and were treated with adjuvant FSRT, delivering 25-36 Gy in 5-6 fractions. Outcomes were computed using Kaplan-Meier survival analysis and univariate analysis.
RESULTS: Fifty-four patients with 63 post-operative cavities were included. Median follow-up was 16 months (3-60). Median metastasis size at diagnosis was 2.9 cm (0.6-8.1) and median planning target volume was 19.7 cm3 (6.3-68.1). Two-year local control (LC) was 83%. When stratified by dose, 2 years LC rate was 95.1% in those treated with 30-36 Gy in 5-6 fractions (BED10 of 48-57.6 Gy10) versus 59.1% lesions treated with 25 Gy in 5 fractions (BED10 of 37.5 Gy10) (p < 0.001). LC was not associated with resection cavity size. One year overall survival was 68.7%, and was independent of BED10. Symptomatic radiation necrosis occurred in 7.9% of patients and was not associated with dose.
CONCLUSION: In the post-operative setting, high-dose FSRT (BED10 > 37.5 Gy10) were associated with a significantly higher rate of LC compared to lower BED regimens. Overall, 25 Gy in 5 fractions is not an adequate dose to control microscopic disease. If selecting a 5-fraction regimen, 30 Gy in five fractions appears to provide excellent tumor bed control.
PMID:31606876 | DOI:10.1007/s11060-019-03308-7
View details for PubMedID 31606876
-
More
-
VMAT and IMRT plan-specific correction factors for linac-based ionization chamber dosimetry Medical physics
Desai VK, Labby ZE, Hyun MA, DeWerd LA, Culberson WS
2019 Feb;46(2):913-924. doi: 10.1002/mp.13293. Epub 2018 Dec 6.
-
More
PURPOSE: The determination of absorbed dose to water from external beam radiotherapy using radiation detectors is currently rooted in calibration protocols that do not account for modulations encountered in patient-specific deliveries. Detector response in composite clinical fields has not been extensively studied due to the time and effort required to determine these corrections on a case-by-case basis. To help bridge this gap in knowledge, corrections for the Exradin A1SL scanning chamber were determined in a large number of composite clinical fields using Monte Carlo methods. The chamber-specific perturbations that contribute the most to the overall correction factor were also determined.
METHODS: A total of 131 patient deliveries comprised of 834 beams from a Varian C-arm linear accelerator were converted to EGSnrc Monte Carlo inputs. A validated BEAMnrc 21EX linear accelerator model was used as a particle source throughout the EGSnrc simulations. Composite field dose distributions were compared against a commercial treatment planning system for validation. The simulation geometry consisted of a cylindrically symmetric water-equivalent phantom with the Exradin A1SL scanning chamber embedded inside. Various chamber perturbation factors were investigated in the egs_chamber user code of EGSnrc and were compared to reference field conditions to determine the plan-specific correction factor.
RESULTS: The simulation results indicated that the Exradin A1SL scanning chamber is suitable to use as an absolute dosimeter within a high-dose and low-gradient target region in most nonstandard composite fields; however, there are still individual cases that require larger delivery-specific corrections. The volume averaging and replacement perturbations showed the largest impact on the overall plan-specific correction factor for the Exradin A1SL scanning chamber, and both volumetric modulated arc therapy (VMAT) and step-and-shoot beams demonstrated similar correction factor magnitudes among the data investigated. Total correction magnitudes greater than 2% were required by 9.1% of step-and-shoot beams and 14.5% of VMAT beams. When examining full composite plan deliveries as opposed to individual beams, 0.0% of composite step-and-shoot plans and 2.6% of composite VMAT plans required correction magnitudes greater than 2%.
CONCLUSIONS: The A1SL scanning chamber was found to be suitable to use for absolute dosimetry in high-dose and low-gradient dose regions of composite IMRT plans but even if a composite dose distribution is large compared to the detector used, a correction-free absorbed dose-to-water measurement is not guaranteed.
PMID:30449040 | DOI:10.1002/mp.13293
View details for PubMedID 30449040
-
More
-
Radiation treatment planning and delivery strategies for a pregnant brain tumor patient Journal of applied clinical medical physics
Labby ZE, Barraclough B, Bayliss RA, Besemer AE, Dunkerley AP, Howard SP
2018 Sep;19(5):368-374. doi: 10.1002/acm2.12262. Epub 2018 Jul 30.
-
More
The management of a pregnant patient in radiation oncology is an infrequent event requiring careful consideration by both the physician and physicist. The aim of this manuscript was to highlight treatment planning techniques and detail measurements of fetal dose for a pregnant patient recently requiring treatment for a brain cancer. A 27-year-old woman was treated during gestational weeks 19-25 for a resected grade 3 astrocytoma to 50.4 Gy in 28 fractions, followed by an additional 9 Gy boost in five fractions. Four potential plans were developed for the patient: a 6 MV 3D-conformal treatment plan with enhanced dynamic wedges, a 6 MV step-and-shoot (SnS) intensity-modulated radiation therapy (IMRT) plan, an unflattened 6 MV SnS IMRT plan, and an Accuray TomoTherapy HDA helical IMRT treatment plan. All treatment plans used strategies to reduce peripheral dose. Fetal dose was estimated for each treatment plan using available literature references, and measurements were made using thermoluminescent dosimeters (TLDs) and an ionization chamber with an anthropomorphic phantom. TLD measurements from a full-course radiation delivery ranged from 1.0 to 1.6 cGy for the 3D-conformal treatment plan, from 1.0 to 1.5 cGy for the 6 MV SnS IMRT plan, from 0.6 to 1.0 cGy for the unflattened 6 MV SnS IMRT plan, and from 1.9 to 2.6 cGy for the TomoTherapy treatment plan. The unflattened 6 MV SnS IMRT treatment plan was selected for treatment for this particular patient, though the fetal doses from all treatment plans were deemed acceptable. The cumulative dose to the patient's unshielded fetus is estimated to be 1.0 cGy at most. The planning technique and distance between the treatment target and fetus both contributed to this relatively low fetal dose. Relevant treatment planning strategies and treatment delivery considerations are discussed to aid radiation oncologists and medical physicists in the management of pregnant patients.
PMID:30062720 | PMC:PMC6123144 | DOI:10.1002/acm2.12262
View details for PubMedID 30062720
-
More
-
A New Era of Image Guidance with Magnetic Resonance-guided Radiation Therapy for Abdominal and Thoracic Malignancies Cureus
Mittauer K, Paliwal B, Hill P, Bayouth JE, Geurts MW, Baschnagel AM, Bradley KA, Harari PM, Rosenberg S, Brower JV, Wojcieszynski AP, Hullett C, Bayliss RA, Labby ZE, Bassetti MF
2018 Apr 4;10(4):e2422. doi: 10.7759/cureus.2422.
-
More
Magnetic resonance-guided radiation therapy (MRgRT) offers advantages for image guidance for radiotherapy treatments as compared to conventional computed tomography (CT)-based modalities. The superior soft tissue contrast of magnetic resonance (MR) enables an improved visualization of the gross tumor and adjacent normal tissues in the treatment of abdominal and thoracic malignancies. Online adaptive capabilities, coupled with advanced motion management of real-time tracking of the tumor, directly allow for high-precision inter-/intrafraction localization. The primary aim of this case series is to describe MR-based interventions for localizing targets not well-visualized with conventional image-guided technologies. The abdominal and thoracic sites of the lung, kidney, liver, and gastric targets are described to illustrate the technological advancement of MR-guidance in radiotherapy.
PMID:29872602 | PMC:PMC5985918 | DOI:10.7759/cureus.2422
View details for PubMedID 29872602
-
More
-
Dosimetric Comparison of Real-Time MRI-Guided Tri-Cobalt-60 Versus Linear Accelerator-Based Stereotactic Body Radiation Therapy Lung Cancer Plans Technology in cancer research & treatment
Wojcieszynski AP, Hill PM, Rosenberg SA, Hullett CR, Labby ZE, Paliwal B, Geurts MW, Bayliss RA, Bayouth JE, Harari PM, Bassetti MF, Baschnagel AM
2017 Jun;16(3):366-372. doi: 10.1177/1533034617691407. Epub 2017 Feb 7.
-
More
PURPOSE: Magnetic resonance imaging-guided radiation therapy has entered clinical practice at several major treatment centers. Treatment of early-stage non-small cell lung cancer with stereotactic body radiation therapy is one potential application of this modality, as some form of respiratory motion management is important to address. We hypothesize that magnetic resonance imaging-guided tri-cobalt-60 radiation therapy can be used to generate clinically acceptable stereotactic body radiation therapy treatment plans. Here, we report on a dosimetric comparison between magnetic resonance imaging-guided radiation therapy plans and internal target volume-based plans utilizing volumetric-modulated arc therapy.
MATERIALS AND METHODS: Ten patients with early-stage non-small cell lung cancer who underwent radiation therapy planning and treatment were studied. Following 4-dimensional computed tomography, patient images were used to generate clinically deliverable plans. For volumetric-modulated arc therapy plans, the planning tumor volume was defined as an internal target volume + 0.5 cm. For magnetic resonance imaging-guided plans, a single mid-inspiratory cycle was used to define a gross tumor volume, then expanded 0.3 cm to the planning tumor volume. Treatment plan parameters were compared.
RESULTS: Planning tumor volumes trended larger for volumetric-modulated arc therapy-based plans, with a mean planning tumor volume of 47.4 mL versus 24.8 mL for magnetic resonance imaging-guided plans ( P = .08). Clinically acceptable plans were achievable via both methods, with bilateral lung V20, 3.9% versus 4.8% ( P = .62). The volume of chest wall receiving greater than 30 Gy was also similar, 22.1 versus 19.8 mL ( P = .78), as were all other parameters commonly used for lung stereotactic body radiation therapy. The ratio of the 50% isodose volume to planning tumor volume was lower in volumetric-modulated arc therapy plans, 4.19 versus 10.0 ( P < .001). Heterogeneity index was comparable between plans, 1.25 versus 1.25 ( P = .98).
CONCLUSION: Magnetic resonance imaging-guided tri-cobalt-60 radiation therapy is capable of delivering lung high-quality stereotactic body radiation therapy plans that are clinically acceptable as compared to volumetric-modulated arc therapy-based plans. Real-time magnetic resonance imaging provides the unique capacity to directly observe tumor motion during treatment for purposes of motion management.
PMID:28168936 | PMC:PMC5616053 | DOI:10.1177/1533034617691407
View details for PubMedID 28168936
-
More
-
Technical Note: Confirming the prescribed angle of CT localizer radiographs and c-arm projection acquisitions Medical physics
Szczykutowicz TP, Labby ZE, Rubert N, Wallace C
2016 Feb;43(2):865-9. doi: 10.1118/1.4940124.
-
More
PURPOSE: Accurate CT radiograph angle is not usually important in diagnostic CT. However, there are applications in radiation oncology and interventional radiology in which the orientation of the x-ray source and detector with respect to the patient is clinically important. The authors present a method for measuring the accuracy of the tube/detector assembly with respect to the prescribed tube/detector position for CT localizer, fluoroscopic, and general radiograph imaging using diagnostic, mobile, and c-arm based CT systems.
METHODS: A mathematical expression relating the x-ray projection of two metal BBs is related to gantry angle. Measurement of the BBs at a prescribed gantry (i.e., c-arm) angle can be obtained and using this relation the prescribed versus actual gantry angle compared. No special service mode or proprietary information is required, only access to projection images is required. Projection images are available in CT via CT localizer radiographs and in the interventional setting via fluorography.
RESULTS: The technique was demonstrated on two systems, a mobile CT scanner and a diagnostic CT scanner. The results confirmed a known issue with the mobile scanner and accurately described the CT localizer angle of the diagnostic system tested.
CONCLUSIONS: This method can be used to quantify gantry angle, which is important when projection images are used for procedure guidance, such as in brachytherapy and interventional radiology applications.
PMID:26843247 | DOI:10.1118/1.4940124
View details for PubMedID 26843247
-
More
-
Gadoxetate for direct tumor therapy and tracking with real-time MRI-guided stereotactic body radiation therapy of the liver Radiotherapy and oncology : journal of the European Society for Therapeutic Radiology and Oncology
Wojcieszynski AP, Rosenberg SA, Brower JV, Hullett CR, Geurts MW, Labby ZE, Hill PM, Bayliss RA, Paliwal B, Bayouth JE, Harari PM, Bassetti MF
2016 Feb;118(2):416-8. doi: 10.1016/j.radonc.2015.10.024. Epub 2015 Nov 25.
-
More
SBRT is increasingly utilized in liver tumor treatment. MRI-guided RT allows for real-time MRI tracking during therapy. Liver tumors are often poorly visualized and most contrast agents are transient. Gadoxetate may allow for sustained tumor visualization. Here, we report on the first use of gadoxetate during real-time MRI-guided SBRT.
PMID:26627702 | DOI:10.1016/j.radonc.2015.10.024
View details for PubMedID 26627702
-
More
-
Dosimetric measurements of an n-butyl cyanoacrylate embolization material for arteriovenous malformations Medical physics
Labby ZE, Chaudhary N, Gemmete JJ, Pandey AS, Roberts DA
2015 Apr;42(4):1739-44. doi: 10.1118/1.4915080.
-
More
PURPOSE: The therapeutic regimen for cranial arteriovenous malformations often involves both stereotactic radiosurgery and endovascular embolization. Embolization agents may contain tantalum or other contrast agents to assist the neurointerventionalists, leading to concerns regarding the dosimetric effects of these agents. This study investigated dosimetric properties of n-butyl cyanoacrylate (n-BCA) plus lipiodol with and without tantalum powder.
METHODS: The embolization agents were provided cured from the manufacturer with and without added tantalum. Attenuation measurements were made for the samples and compared to the attenuation of a solid water substitute using a 6 MV photon beam. Effective linear attenuation coefficients (ELAC) were derived from attenuation measurements made using a portal imager and derived sample thickness maps projected in an identical geometry. Probable dosimetric errors for calculations in which the embolized regions are overridden with the properties of water were calculated using the ELAC values. Interface effects were investigated using a parallel plate ion chamber placed at set distances below fixed samples. Finally, Hounsfield units (HU) were measured using a stereotactic radiosurgery CT protocol, and more appropriate HU values were derived from the ELAC results and the CT scanner's HU calibration curve.
RESULTS: The ELAC was 0.0516 ± 0.0063 cm(-1) and 0.0580 ± 0.0091 cm(-1) for n-BCA without and with tantalum, respectively, compared to 0.0487 ± 0.0009 cm(-1) for the water substitute. Dose calculations with the embolized region set to be water equivalent in the treatment planning system would result in errors of -0.29% and -0.93% per cm thickness of n-BCA without and with tantalum, respectively. Interface effects compared to water were small in magnitude and limited in distance for both embolization materials. CT values at 120 kVp were 2082 and 2358 HU for n-BCA without and with tantalum, respectively; dosimetrically appropriate HU values were estimated to be 79 and 199 HU, respectively.
CONCLUSIONS: The dosimetric properties of the embolization agents are very close to those of water for a 6 MV beam. Therefore, treating the entire intracranial space as uniform in composition will result in less than 1% dosimetric error for n-BCA emboli smaller than 3.4 cm without added tantalum and n-BCA emboli smaller than 1.1 cm with added tantalum. Furthermore, when effective embolization can be achieved by the neurointerventionalist using n-BCA without tantalum, the dosimetric impact of overriding material properties will be lessened. However, due to the high attenuation of embolization agents with and without added tantalum for diagnostic energies, artifacts may occur that necessitate additional imaging to accurately identify the spatial extent of the region to be treated.
PMID:25832063 | DOI:10.1118/1.4915080
View details for PubMedID 25832063
-
More
-
CT-based pulmonary artery measurements for the assessment of pulmonary hypertension Academic radiology
Corson N, Armato SG, Labby ZE, Straus C, Starkey A, Gomberg-Maitland M
2014 Apr;21(4):523-30. doi: 10.1016/j.acra.2013.12.015.
-
More
RATIONALE AND OBJECTIVES: Pulmonary hypertension (PH) is a complex and fatal disease that is difficult to diagnose noninvasively. This study evaluated previously published computed tomography-based vessel measurement criteria and investigated the predictive power and diagnostic ability of the main pulmonary artery diameter (MPAD) and the ratio of MPAD to aorta diameter (rPA).
MATERIALS AND METHODS: The database for this study consisted of 175 PH patients (for whom mean pulmonary artery pressure [mPAP] was known), 16 patients without PH but with known mPAP (non-PH patients), and 114 "normal" patients without known mPAP. The performance of previously published criteria, MPAD > 29 mm and rPA > 1, was determined. The relationship between vessel measurements and mPAP was evaluated through correlation and linear regression analysis. The ability of these measurements to discriminate between patients with and without PH was determined by receiver operating characteristic analysis.
RESULTS: For discriminating between PH and "normal" patients, the sensitivity and specificity of the criterion MPAD > 29 mm were 0.89 (0.84-0.93) and 0.83 (0.76-0.90), respectively, and the sensitivity and specificity of the criterion rPA > 1 were 0.89 (0.85-0.94) and 0.82 (0.74-0.89), respectively. At a specificity of 0.95 in the task of separating PH and "normal" patients, the sensitivity of MPAD was 0.81 (0.72-0.90) and the sensitivity of rPA was 0.76 (0.66-0.85), but the specificity for both decreased when non-PH patients were included. For the combined PH and non-PH patient groups, the correlation between the vessel measurements and mPAP was significant but low, and the ability of the vessel measurements to predict mPAP was limited.
CONCLUSION: This study found that the sensitivity of previously published vessel criteria for identifying PH patients is high, but the specificity may not be high enough for routine use in a clinical patient population.
PMID:24594422 | PMC:PMC3985437 | DOI:10.1016/j.acra.2013.12.015
View details for PubMedID 24594422
-
More
-
Imaging in pleural mesothelioma: a review of the 11th International Conference of the International Mesothelioma Interest Group Lung cancer (Amsterdam, Netherlands)
Armato SG, Labby ZE, Coolen J, Klabatsa A, Feigen M, Persigehl T, Gill RR
2013 Nov;82(2):190-6. doi: 10.1016/j.lungcan.2013.08.005. Epub 2013 Aug 15.
-
More
Imaging of malignant pleural mesothelioma (MPM) is essential to the diagnosis, assessment, and monitoring of this disease. The complex morphology and growth pattern of MPM, however, create unique challenges for image acquisition and interpretation. These challenges have captured the attention of investigators around the world, some of whom presented their work at the 2012 International Conference of the International Mesothelioma Interest Group (iMig 2012) in Boston, Massachusetts, USA, September 2012. The measurement of tumor thickness on computed tomography (CT) scans is the current standard of care in the assessment of MPM tumor response to therapy; in this context, variability among observers in the measurement task and in the tumor response classification categories derived from such measurements was reported. Alternate CT-based tumor response criteria, specifically direct measurement of tumor volume change and change in lung volume as a surrogate for tumor response, were presented. Dynamic contrast-enhanced CT has a role in other settings, but investigation into its potential use for imaging mesothelioma tumor perfusion only recently has been initiated. Magnetic resonance imaging (MRI) and positron-emission tomography (PET) are important imaging modalities in MPM and complement the information provided by CT. The pointillism sign in diffusion-weighted MRI was reported as a potential parameter for the classification of pleural lesions as benign or malignant, and PET parameters that measure tumor activity and functional tumor volume were presented as indicators of patient prognosis. Also reported was the use of PET/CT in the management of patients who undergo high-dose radiation therapy. Imaging for MPM impacts everything from initial patient diagnosis to the outcomes of clinical trials; iMig 2012 captured this broad range of imaging applications as investigators exploit technology and implement multidisciplinary approaches toward the benefit of MPM patients.
PMID:24018024 | DOI:10.1016/j.lungcan.2013.08.005
View details for PubMedID 24018024
-
More
-
Variability of tumor area measurements for response assessment in malignant pleural mesothelioma Medical physics
Labby ZE, Straus C, Caligiuri P, MacMahon H, Li P, Funaki A, Kindler HL, Armato SG
2013 Aug;40(8):081916. doi: 10.1118/1.4810940.
-
More
PURPOSE: The measurement of malignant pleural mesothelioma is critical to the assessment of tumor response to therapy. Current response assessment standards utilize summed linear measurements acquired on three computed tomography (CT) sections. The purpose of this study was to evaluate manual area measurements as an alternate response assessment metric, specifically through the study of measurement interobserver variability.
METHODS: Two CT scans from each of 31 patients were collected. Using a computer interface, five observers contoured tumor on three selected CT sections from each baseline scan. Four observers also constructed matched follow-up scan tumor contours for the same 31 patients. Area measurements extracted from these contours were compared using a random effects analysis of variance model to assess relative interobserver variability. The sums of section area measurements were also analyzed, since these area sums are more clinically relevant for response assessment.
RESULTS: When each observer's measurements were compared with those of the other four observers, strong correlation was observed. The 95% confidence interval for relative interobserver variability of baseline scan summed area measurements was [-71%, +240%], spanning 311%. For the follow-up scan summed area measurements, the 95% confidence interval for relative interobserver variability was [-41%, +70%], spanning 111%. At both baseline and follow-up, the variability among observers was a significant component of the total variability in both per-section and summed area measurements (p<0.0001).
CONCLUSIONS: Despite the ability of tumor area measurements to capture tumor burden with greater fidelity than linear tumor thickness measurements, manual area measurements may not be a robust means of response assessment in mesothelioma patients.
PMID:23927330 | PMC:PMC3739828 | DOI:10.1118/1.4810940
View details for PubMedID 23927330
-
More
-
Lung volume measurements as a surrogate marker for patient response in malignant pleural mesothelioma Journal of thoracic oncology : official publication of the International Association for the Study of Lung Cancer
Labby ZE, Armato SG, Dignam JJ, Straus C, Kindler HL, Nowak AK
2013 Apr;8(4):478-86. doi: 10.1097/JTO.0b013e31828354c8.
-
More
INTRODUCTION: The purpose of this study was to investigate the continuous changes in three distinct response assessment methods during treatment as a marker of response for patients with mesothelioma. Linear tumor thickness measurements, disease volume measurements, and lung volume measurements (a physiological correlate of disease volumes) were investigated in this study.
METHODS: Serial computed tomography scans were obtained during the course of clinically standard chemotherapy for 61 patients. For each of the 216 computed tomography scans, the aerated lung volumes were segmented using a fully automated method, and the pleural disease volume was segmented using a semiautomated method. Modified Response Evaluation Criteria in Solid Tumors linear-thickness measurements were acquired clinically. Diseased (ipsilateral) lung volumes were normalized by the respective contralateral lung volumes to account for the differences in inspiration between scans for each patient. Relative changes in each metric from baseline were tracked over the course of follow-up imaging. Survival modeling was performed using Cox proportional hazards models with time-varying covariates.
RESULTS: Median survival from pretreatment baseline imaging was 12.7 months. A negative correlation was observed between measurements of lung volume and disease volume, and a positive correlation was observed between linear-thickness measurements and disease volume. As continuous numerical parameters, all three response assessment methods were significant imaging biomarkers of patient prognosis in independent survival models.
CONCLUSIONS: Analysis of trajectories of linear-thickness measurements, disease volume measurements, and lung volume measurements during chemotherapy for patients with mesothelioma indicates that increasing linear thickness, increasing disease volume, and decreasing lung volume are all significantly and independently associated with poor patient prognosis.
PMID:23486268 | PMC:PMC3597989 | DOI:10.1097/JTO.0b013e31828354c8
View details for PubMedID 23486268
-
More
-
Disease volumes as a marker for patient response in malignant pleural mesothelioma Annals of oncology : official journal of the European Society for Medical Oncology
Labby ZE, Nowak AK, Dignam JJ, Straus C, Kindler HL, Armato SG
2013 Apr;24(4):999-1005. doi: 10.1093/annonc/mds535. Epub 2012 Nov 8.
-
More
BACKGROUND: The goal of this study was to create a comprehensive model for malignant pleural mesothelioma patient survival utilizing continuous, time-varying estimates of disease volume from computed tomography (CT) imaging in conjunction with clinical covariates.
PATIENTS AND METHODS: Serial CT scans were obtained during the course of clinically standard chemotherapy for 81 patients. The pleural disease volume was segmented for each of the 281 CT scans, and relative changes in disease volume from the baseline scan were tracked over the course of serial follow-up imaging. A prognostic model was built using time-varying disease volume measurements in conjunction with clinical covariates.
RESULTS: Over the course of treatment, disease volume decreased by an average of 19%, and median patient survival was 12.6 months from baseline. In a multivariate survival model, changes in disease volume were significantly associated with patient survival along with disease histology, Eastern Cooperative Oncology Group performance status, and presence of dyspnea.
CONCLUSIONS: Analysis of the trajectories of disease volumes during chemotherapy for patients with mesothelioma indicates that increasing disease volume was significantly and independently associated with poor patient prognosis in both univariate and multivariate survival models.
PMID:23144443 | PMC:PMC3603437 | DOI:10.1093/annonc/mds535
View details for PubMedID 23144443
-
More
-
Optimization of response classification criteria for patients with malignant pleural mesothelioma Journal of thoracic oncology : official publication of the International Association for the Study of Lung Cancer
Labby ZE, Armato SG, Kindler HL, Dignam JJ, Hasani A, Nowak AK
2012 Nov;7(11):1728-34. doi: 10.1097/JTO.0b013e318269fe21.
-
More
INTRODUCTION: Response-assessment metrics play an important role in clinical trials and routine patient management. For patients with malignant pleural mesothelioma (MPM), the standard for response assessment is image-based measurements of tumor thickness made according to the modified RECIST (Response Evaluation Criteria in Solid Tumors) protocol. To classify tumor response, changes in tumor thickness are compared with the standard RECIST -30% and +20% cutoffs for partial response (PR) and progressive disease (PD), respectively, which are not specific to MPM. The purpose of this work is to optimize the correlation between tumor response and patient survival by assessing the validity of existing response criteria in MPM and proposing alternative criteria.
METHODS: Computed tomography measurements of tumor thickness were acquired at baseline and throughout treatment for 78 patients undergoing standard-of-care chemotherapy. Overall survival was correlated with best response and first follow-up response using Harrell's C statistic. The response criteria for PD and PR were each varied in 1% increments to obtain optimized classification criteria. The performance was cross-validated using a leave-one-out approach.
RESULTS: Median survival was 14.9 months. The performance of the standard RECIST criteria in correlating response with survival was C=0.778, whereas the optimized performance of C=0.855 was obtained with criteria of -64% for PR and +50% for PD. After cross-validation, this performance was slightly reduced to C=0.829.
CONCLUSIONS: Optimized tumor-response classification criteria were obtained for patients with MPM. These criteria improve the correlation between image-based response and patient survival.
PMID:23059782 | PMC:PMC3473122 | DOI:10.1097/JTO.0b013e318269fe21
View details for PubMedID 23059782
-
More
-
Lung texture in serial thoracic CT scans: assessment of change introduced by image registration Medical physics
Cunliffe AR, Al-Hallaq HA, Labby ZE, Pelizzari CA, Straus C, Sensakovic WF, Ludwig M, Armato SG
2012 Aug;39(8):4679-90. doi: 10.1118/1.4730505.
-
More
PURPOSE: The aim of this study was to quantify the effect of four image registration methods on lung texture features extracted from serial computed tomography (CT) scans obtained from healthy human subjects.
METHODS: Two chest CT scans acquired at different time points were collected retrospectively for each of 27 patients. Following automated lung segmentation, each follow-up CT scan was registered to the baseline scan using four algorithms: (1) rigid, (2) affine, (3) B-splines deformable, and (4) demons deformable. The registration accuracy for each scan pair was evaluated by measuring the Euclidean distance between 150 identified landmarks. On average, 1432 spatially matched 32 × 32-pixel region-of-interest (ROI) pairs were automatically extracted from each scan pair. First-order, fractal, Fourier, Laws' filter, and gray-level co-occurrence matrix texture features were calculated in each ROI, for a total of 140 features. Agreement between baseline and follow-up scan ROI feature values was assessed by Bland-Altman analysis for each feature; the range spanned by the 95% limits of agreement of feature value differences was calculated and normalized by the average feature value to obtain the normalized range of agreement (nRoA). Features with small nRoA were considered "registration-stable." The normalized bias for each feature was calculated from the feature value differences between baseline and follow-up scans averaged across all ROIs in every patient. Because patients had "normal" chest CT scans, minimal change in texture feature values between scan pairs was anticipated, with the expectation of small bias and narrow limits of agreement.
RESULTS: Registration with demons reduced the Euclidean distance between landmarks such that only 9% of landmarks were separated by ≥1 mm, compared with rigid (98%), affine (95%), and B-splines (90%). Ninety-nine of the 140 (71%) features analyzed yielded nRoA > 50% for all registration methods, indicating that the majority of feature values were perturbed following registration. Nineteen of the features (14%) had nRoA < 15% following demons registration, indicating relative feature value stability. Student's t-tests showed that the nRoA of these 19 features was significantly larger when rigid, affine, or B-splines registration methods were used compared with demons registration. Demons registration yielded greater normalized bias in feature value change than B-splines registration, though this difference was not significant (p = 0.15).
CONCLUSIONS: Demons registration provided higher spatial accuracy between matched anatomic landmarks in serial CT scans than rigid, affine, or B-splines algorithms. Texture feature changes calculated in healthy lung tissue from serial CT scans were smaller following demons registration compared with all other algorithms. Though registration altered the values of the majority of texture features, 19 features remained relatively stable after demons registration, indicating their potential for detecting pathologic change in serial CT scans. Combined use of accurate deformable registration using demons and texture analysis may allow for quantitative evaluation of local changes in lung tissue due to disease progression or treatment response.
PMID:22894392 | PMC:PMC3411586 | DOI:10.1118/1.4730505
View details for PubMedID 22894392
-
More
-
Broadband, high-resolution spatial heterodyne spectrometer Applied optics
Lawler JE, Labby ZE, Harlander JM, Roesler FL
2008 Dec 1;47(34):6371-84. doi: 10.1364/ao.47.006371.
-
More
Design and performance parameters for a broadband, high-resolution spatial heterodyne spectrometer (SHS) are reported. The Mark 1 SHS achieves more than a factor of 5 in continuous wavenumber coverage with a design resolving power in the hundreds of thousands.
PMID:19037365 | DOI:10.1364/ao.47.006371
View details for PubMedID 19037365
-
More
Contact Information
Zacariah Labby, PhD
4621 Eastpark Blvd,K4/b100
Madison, WI 53718
