 Our two-year residency program features numerous well-defined rotations to ensure a complete, high-quality training curriculum for our physics residents. Additionally, we integrate our residents into all facets of clinical practice. Explore the specifics of our program structure below.
Our two-year residency program features numerous well-defined rotations to ensure a complete, high-quality training curriculum for our physics residents. Additionally, we integrate our residents into all facets of clinical practice. Explore the specifics of our program structure below.
This is an accordion element with a series of buttons that open and close related content panels.
Welcome
Program Structure
About the Department
Current and Former Residents
Admissions Process
Contact Us
Clinical Rotations
This is an accordion element with a series of buttons that open and close related content panels.
Orientation (0.5 mo)
The goal of this rotation is for residents to get oriented to the department and residency program. The resident will complete various shadowing assignments and projects designed to help them get acquainted with the various team members, clinical workflows, treatment machines, software, and other equipment that the resident is going to be working with over the next two years. Residents will also participate in two rotation “projects” including (1) following a single patient all the way through the carepath from consult to treatment and (2) performing an end-to-end phantom test from CT simulation to treatment that will allow the resident hands-on experience with various equipment and software’s.
Mentor: Abby Besemer

Linacs and Detectors (1.5 mo)
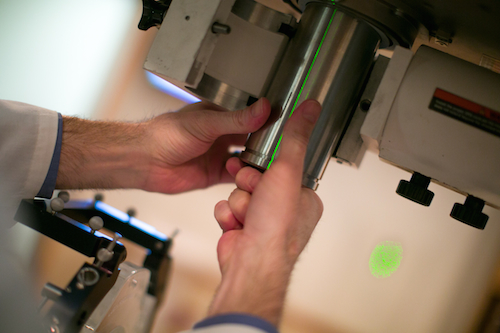
This rotation is designed to introduce the resident to a typical “c-arm” treatment delivery system, e.g., the Varian TrueBeam platform. The resident will learn about the therapeutic beam production and shaping aspects of the system, along with the potential failure modes of the system. The resident will learn and perform national and departmental standards for periodic and post-repair quality assurance testing.
Residents will also learn about the available detectors used to measure radiation in the field of radiation oncology. The rotation will cover the functionality and application of each device. Residents will also be given the opportunity to learn about dosimeter calibrations from the University of Wisconsin Accredited Dosimetry Calibration Laboratory.
Mentors: Lindsay Zammit, Alison Arnold, Autumn Walter-Denzin, Jessica Miller


Basic Treatment Planning (2.5 mo)
During the basic treatment planning rotation, residents will learn treatment planning techniques for 2D and 3D conformal radiation therapy for a wide variety of treatment sites. Residents will also learn the physics of treatment planning and dose calculation to help further their understanding of the treatment planning process. Finally, residents will participate in CT simulation, treatment planning and plan review for UWHealth patients.
Mentors: Gemma Davies, Patrick Hill, and Alyx Alfson



Advanced Treatment Planning (3.5 mo)
During this rotation, the resident builds upon the expertise gained during the Basic Treatment Planning rotation by extending focus to IMRT, VMAT, and TomoTherapy treatment plan design. Additionally, the resident learns about IMRT QA program management, modern treatment plan optimization strategies, and updated clinical treatment planning goals and constraints.
Mentors: Adam Bayliss, Dustin Jacqmin, and Alyx Alfson


Imaging and MRI guided Radiation Therapy (MRgRT) (3 mo)
First, the resident will focus on understanding the physics behind the imaging techniques commonly used for Radiation Oncology patients, as well as understanding the applications of these images, both during treatment planning and treatment delivery. Image acquisition, image processing, image quality, and image registration and fusion are covered for common modalities such as 2D projection images, CT, MR, Ultrasound, PET, and non-ionizing imaging techniques.
During the later part of the rotation, residents will learn about the characteristics of both MRI-guided radiation therapy (MRgRT) delivered via a low-field MR-linac and MRI simulation (i.e., imaging of patients in the treatment position). Major competencies will include MRI safety, quality assurance (QA), and evaluating the impact of the magnetic field on both dosimetry and image quality parameters. Imaging sequences, artifacts, and use cases will be highlighted. Residents will actively participate in the machine and patient-specific QA processes and become acquainted with MR-guided adaptive radiation therapy, including MR-only treatment planning. Specific staffing and equipment needs in these hybrid environments will be demonstrated. Overall, this rotation features state of the art equipment for cancer care and builds upon the unique strengths in MRI and MRgRT at the University of Wisconsin-Madison.
Mentor: Michael Lawless, Carri Glide-Hurst, and Andrew Shepard

Radiosurgery (2.5 mo)
On the stereotactic radiosurgery rotation, residents will learn about available treatment techniques used in the delivery of high dose-per-fraction, highly conformal radiation plans. Residents will also learn about appropriate procedures in the commissioning of small-field treatment techniques as well as the specifics of small-field dosimetry. Finally, residents will participate in radiosurgery planning and delivery for UWHealth patients.
Mentors: Zac Labby, Sharareh Fakhraei


Brachytherapy (3 mo)
During the brachytherapy rotation, residents will learn the procedures, quality assurance and regulations for all brachytherapy procedures performed at the University of Wisconsin Hospital and Clinics. Residents will be able to create clinical treatment plans for high dose rate and low dose rate applications. After the completion of this rotation, the resident should have the skills and knowledge necessary to be able to create a safe, efficient and effective clinical brachytherapy program at another institution.
Mentors: Charles Wallace, Jordan Slagowski


Proton Therapy (1 mo)
During the proton therapy rotation, residents will learn the fundamental physics of proton therapy and participate in the clinical proton therapy processes including simulation, treatment planning, treatment, image guidance, and quality assurance activities. The resident will get hands-on experience working with a pencil beam scanning gantry-based system as well as our fixed beam and novel upright chair and CT imaging system.
Mentors: Minglei Kang, Shannon O’Reilly

Special Topics (2 mo)
On this rotation residents first learn about several specialized topics in radiation therapy including total body irradiation (TBI), total marrow irradiation (TMI), craniospinal irradiation (CSI), total-skin electron therapy (TSET), out of field dose, and the management of pregnant patients and patients with cardiac implantable electronic devices (CIEDs), theranostics and radiopharmaceutical therapy, clinical trials, informatics, professionalism, leadership, ethics, patient communication, and global health.
Mentors: Abby Besemer

Commissioning, Beam Modeling, and Shielding (3 mo)
During the commissioning rotation, residents will learn about the process of installing a new linear accelerator, including selection and performance specification, acceptance testing, and commissioning. The resident will participate in beam data acquisition measurements for a new linear accelerator. Residents will also learn about the methods used for commissioning other radiotherapy devices and will be responsible for a commissioning project of their own.
On this rotation, residents will also learn about the selection, implementation, utilization, and management of Treatment Planning Systems. This includes configuring machines and beam model parameter values, use of physics and planning modules, commissioning, as well as establishing and maintaining quality assurance. Residents will use measured beam data and create their own validated commissioned machine.
This rotation also explores the latest methods for performing shielding calculations and places an emphasis on practicing these methods through a series of common radiation therapy shielding scenarios. Other facility design goals, including room layout, construction cost management, electrical/HVAC considerations, and radiation surveys will also be discussed.
Mentors: Eric Wallat, Sean Frigo, Jennie Crosby, and Zac Labby



Clinical Practicum (Longitudinal 2 year rotation)
The clinical practicum is a longitudinal rotation that takes place over the full 24 months of the residency program. The rotation will cover all the clinical tasks that residents will be expected to participate in on a routine basis. These tasks include monthly, annual, and post-service linac and CT QA, patient-specific IMRT QA for the linacs/tomo and ViewRay, treatment planning, plan reviews, weekly chart checks, and other physicist of the day (POD) tasks. The goal is to provide residents with a chance to complete these tasks as independently as possible, allowing them to gradually build both technical proficiency and clinical judgment under the supervision of experienced faculty. As residents progress, they are encouraged to take increasing ownership of clinical responsibilities, reinforcing confidence and competence in preparation for independent clinical practice.
Mentors: Chingyun Cheng (CC), Abby Besemer

LEADER (Longitudinal 2 year rotation)
The Longitudinal Research & Clinical Project Development Rotation (LEADER) is a longitudinal rotation that takes place over the full 24 months of the residency program. LEADER will provide trainees the opportunity to build their practice quality improvement, research, and technical communication skills, by leading an innovative quality improvement or clinical research project with the support of a DHO mentor. This longitudinal rotation requires the resident complete a major clinical development or research project under the direct supervision of a DHO faculty member. At the conclusion of the project, the resident will have disseminated the results and conclusions of their work by presentation at a scientific conference.
Mentor: Jordan Slagowski

Integrated Clinical Activities
Physics residents have the opportunity to contribute to clinical services in a variety of areas after residents have demonstrated competency. Examples include:
-
Quasi-independent clinical coverage
-
Shadowing clinical physicists on a rotating basis
-
Unique patient consultations
-
Acquisition and processing of patient 4DCT and Respiratory-Gated Simulation Data
-
Weekly patient chart review
-
External Beam clinical patient planning
-
Brachytherapy clinical patient planning
-
Monthly Quality Assurance of Linear Accelerators
-
Independent measurement of IMRT Delivery QA plans
-
Preparing and managing the display of patient data for departmental Chart Rounds
-
Brachytherapy HDR Remote Afterloader Daily QA
-
Various clinical projects, including device and procedure commissioning measurements
Cross-Institutional Training
One exciting and unique aspect of our program is that residents have the opportunity to interact with residents at other institutions through various cross-institutional initiatives. These programs are a great way for residents to connect with others in the field and learn about different technologies, workflows, and cultures outside of their own institution. For example, our program participates in the following programs:
- Multi-Institutional Career Development Program: Residents meet monthly with residents from several other programs to learn about topics related to networking, applying for jobs, interviewing, career development, etc. The meetings feature discussions with expert faculty physicists from all across the country and interactive workshops where residents can participate in mock interviews and get immediate feedback on CVs and cover letters.
- AAPM Multi-institutional Journal Club: Residents meet approximately every other month with residents from several other programs to present and discuss journal articles of their choosing. The informal discussions with other residents are a great way to learn about how practices vary across different institutions.
- Resident Away Rotation: Last year we were able have one of our residents participate in a 1 week away rotation at the University of Colorado where they participated in GammaKnife a source exchange. Our efforts creating the framework for a resident away rotation were presented in the “Arthur Boyer Award for Innovation in Medical Physics Education” session at the 2023 AAPM meeting. We are hopeful that we can offer the opportunity for more away rotations in the future, if funding allows.
Resident Assessment
After each rotation, residents will be given an oral exam with two components: “quick response” questions, where each question is limited in scope and the answer must be provided in a timed manner (usually five minutes) and “free-form” questions that are designed to probe the depth of the resident’s knowledge in a given area.
The “quick response” questions are designed to encourage the resident to smoothly and efficiently demonstrate an understanding of the examined topic without getting lost in excessive detail and to prepare the resident for similar question formats found on certification exams.
The “quick response” and “free-form” questions are scored separately, and the resident must pass both portions of the exam before advancing to the next rotation.
Program Oversight
The Radiation Oncology Physics Residency Program is directed by the program director and associate director and is overseen by the Residency Program Oversight Committee. The oversight committee reviews the program at least annually and makes recommendations for improvements to the directors. Through this leadership, our program conscientiously and actively seeks opportunities to make our training program one of the best programs available in clinical radiation oncology physics.
Number of Residents
The Radiation Oncology Physics Residency Program is designed to enroll 3 new residents every July with a total of 6 residents in the program.
Compensation and Benefits
Medical physics residents receive benefits commensurate with medical residents. These include:
- 2025-2026 salary: $66,149 (PGY-1) and $72,236 (PGY-2)
- $2500 per year conference travel fund. Any unused funds can be used to purchase education materials, pay dues, etc
- Comprehensive health coverage, dental, vision, and various forms of life insurance
- PTO:
- 13 vacation days per year
- 12 sick days per year
- 9 holidays per year (become floating if holiday is on the weekend)
- 8 conference days
- 5 comp days following Anual QAs
- Residents can request to work from home on days that they do not have any clinical duties or onsite rotation activities
- Laptops with built in webcam, capable of full remote access while working offsite
- Lab coats, scrubs, and pagers provided by the University at the beginning of residency. Laundering is provided free of charge.
The University of Wisconsin-Madison is an Equal Opportunity Employer
Qualified applicants will receive consideration for employment without regard to, including but not limited to, race, color, religion, sex, sexual orientation, national origin, age, pregnancy, disability, or status as a protected veteran and other bases as defined by federal regulations and UW System policies. We promote excellence by acknowledging skills and expertise from all backgrounds and encourage all qualified individuals to apply.
